Since its inception United Ostomy Associations of America, Inc (UOAA) has supported and welcomed members living with a urostomy (ileal conduit) or urinary diversion as a result of bladder cancer and related conditions.
May is Bladder Cancer Awareness Month. The American Cancer Society’s estimates about 82,290 new cases of bladder cancer United States for 2023 and about 16,710 deaths from bladder cancer (about 12,160 in men and 4,550 in women)
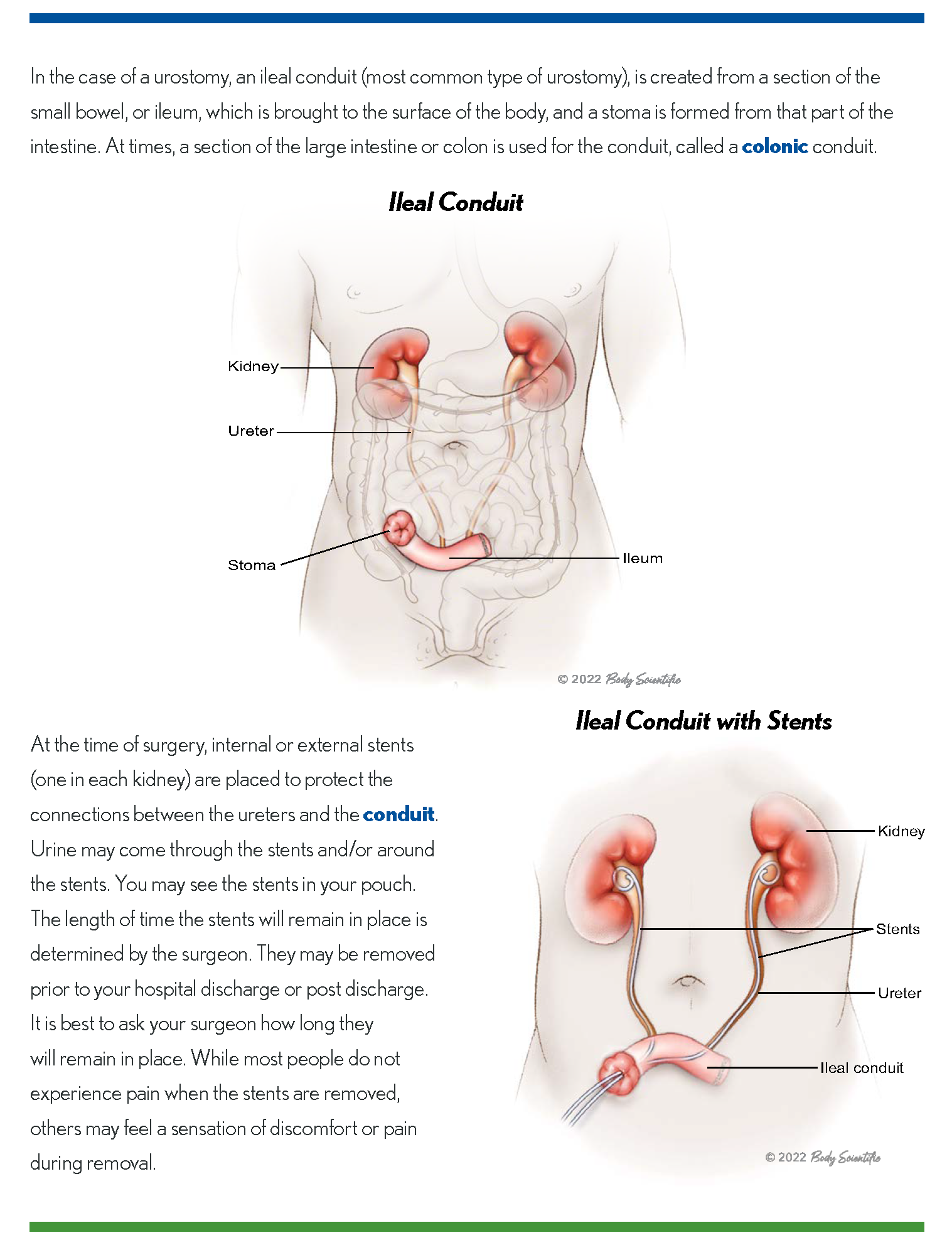
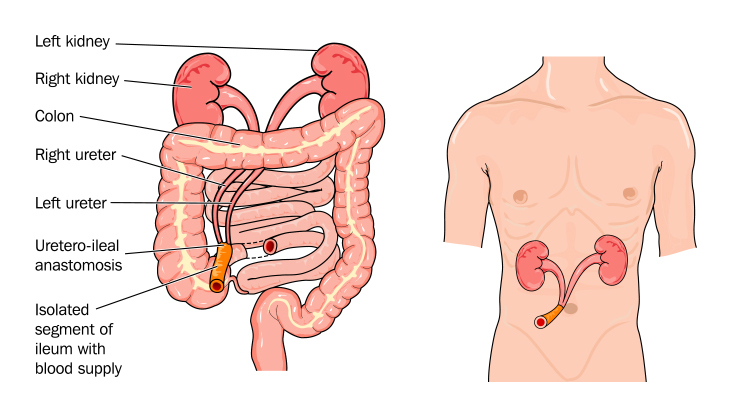
While this common cancer is most often treated without radical surgery a urologist may suggest bladder removal surgery to stop the cancer if a bladder tumor reaches the deeper muscle wall or resists other therapy. A urinary diversion is needed to replace the bladder. This involves using parts of the intestines to allow urine to pass from the kidneys to either an internal urinary reservoir pouch such as Indiana Pouch or a neobladder or an external ileal conduit, when a stoma is formed. An ostomy pouch is worn over the stoma to collect urine.
With surgery comes new things to learn and adjust to in order to achieve the quality of life you were used to before bladder cancer.
UOAA has over 270 Affiliated Support Groups around the United States. Bladder cancer survivors attend many of them and also serve as volunteers and leaders. Peer support and preparation can put you on the path to success in what may be a challenging time both emotionally and physically.
We recognize that those with an ileostomy, colostomy and various gastrointestinal disorders may dominate public conversations and education about living with an ostomy. Please know that the voices of urostomates and those with a urinary diversion are also supported and amplified by UOAA.
A new Living with a Urostomy Guide was launched this year and is available for free online. Created by ostomy nurses with input from a urostomy patient and a leading urologist, this trusted resource is vital to anyone who has or may have to have this life-saving surgery.
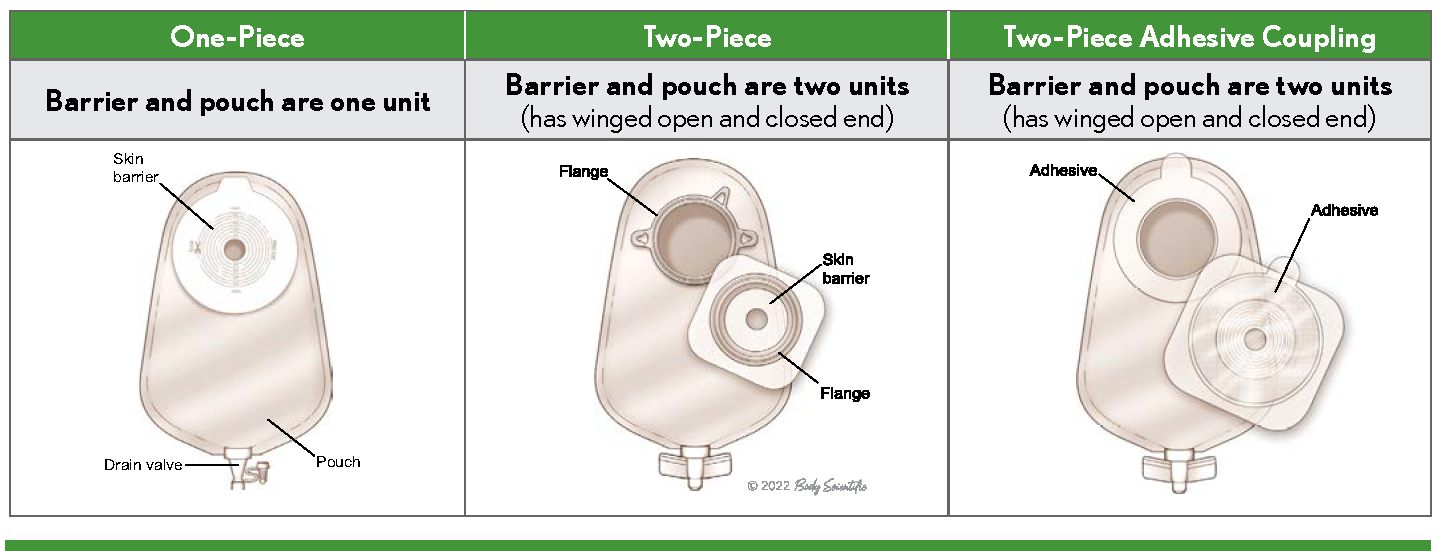
Learn about the unique aspects of a urostomy pouch and options that help improve sleep for urostomates like a night drainage bag.
Ostomy.org is also home to a guide on continent urostomies and other specific considerations.
UOAA advocates on a national level for all people living with an ostomy or continent diversion. Consider taking out a National Individual Membership to help amplify our voices and receive special member benefits along the way.
Check out our many self-advocacy tools designed to help you know what to expect and to take control of your healthcare. Learn that you matter and become a champion for the Ostomy and Continent Diversion Patient Bill of Rights.
It’s important to learn the facts about living with an ostomy. After the healing period outlined by your surgeon you can swim, bathe, travel, and embrace a new normal life. Reading patient stories from both the male urostomy patient and female bladder cancer survivor perspectives are also helpful.
Seize any opportunity to meet other urostomates. UOAA’s 2023 National Conference in August will feature special sessions and meet-up opportunities for people living with a urostomy.
People living with an urostomy as a result of bladder cancer may experience unique sexual issues. Consult with you doctor but also learn about some common issues in our sexuality and intimacy guide.
Misinformation and stigmas surrounding both ostomy surgery and bladder cancer still exist. Nonprofits like Bladder Cancer Advocacy Network (BCAN) and UOAA are working to improve quality of life with support and information. Bladder cancer survivors are an important part of UOAA, join with us to create a better tomorrow.

 Why Do People Need A Urostomy?
Why Do People Need A Urostomy?
 So, what can I do now that I have a urostomy?
So, what can I do now that I have a urostomy? There are so many other things I have been able to do since my
There are so many other things I have been able to do since my 
