Among the general public there is still a perception that people living with an “ostomy bag” or pouch are older seniors or at least middle-aged. Those searching on social media however will soon discover that younger people with an ostomy are not only visible, but sharing and embracing “ostomy life” in a whole new way.

Allison Rosen and friends at the Waterwall Park close to the Royal Sonesta Houston Galleria, the site of the UOAA 2023 National Conference.
Many young adults with an ostomy have never had the opportunity to meet another person they could truly relate to.
What if there was a place where online ostomy friends could meet in person, socialize, laugh, cry and just be together? Well, that place is UOAA’s National Conference August 10-12, 2023 in Houston, Texas.
Attendees of all ages will get to experience a large ostomy product exhibit hall and sign-up to sample products and see a WOC nurse at the free stoma clinic. Former Miss Texas and current J-Poucher Magen Cherry will provide the keynote welcome.
Ostomy experts will also speak and be on hand to answer surgery-specific questions for people with an ileostomy, colostomy, urostomy, j-pouch or continent diversion. Young adults, along with Caregivers, IBD Patients, LGBTQ+, and kids/parents will be offered even more specialized sessions and tracks.
Young Adult Track
After its successful debut in Philadelphia, the Young Adult Track is back for this year’s conference! Designed for ostomates in an earlier stage of life, the track features topics like, dating and sexuality, body image, managing school/work, navigating parenthood, exercise, and staying active all while juggling ostomy care and other chronic health conditions.
Sessions range from formal presentations and panel discussions to off-the-cuff conversations and opportunities to connect with fellow young ostomates. The Young Adult Track offers participants the opportunity to learn new things while forming friendships and bonds that extend well beyond the weekend of the conference.
”If you’re looking for peers in your age range who truly “get it,” look no further — we can’t wait to see you in Houston!” says co-organizer Molly Atwater-Pulisic (Molly Olly Ostomy). The young adult group typically meet informally after hours in the hotel lounge and go on city outings together as well.
You’ll want to stay at the Royal Sonesta Houston Galleria to not miss out and be close to all the action. A special UOAA group rate is available.
The young adult track is awesome, because we make fast friends and are able to relax and talk openly and casually about personal, ostomy-related topics that are sometimes difficult to share with people in our usual daily lives. -Nate Hadlock

Local Houstonian and ostomy advocate Allison Rosen is helping to plan a Texas themed evening of line dancing, drinks and desserts. “I am looking forward to meeting virtual Ostomy friends in person for the first time! Meeting others who understand I know will be life changing!” Rosen says.
Young Adult Track attendees will have a dedicated meeting room starting with a meet and greet on the morning of Thursday, August 10 ending with FAQs Saturday afternoon before the closing party. A special Friday night gathering just for the Young Adults is also being planned with track sponsor Hollister.
If this all feels a bit overwhelming don’t worry you’ll be embraced with open arms. Unofficial social chair Alyssa Zeldenrust has made it her mission to greet and connect young ostomates since first attending the conference in 2011. In a testimonial video she shares why she keeps coming back. “All of us are on our second chance at life, so it’s extra special to all be together and it’s a very joyous atmosphere.”
She’ll also be speaking on Ostomy FAVE Things along with other conference veterans Chloe Moody and Nate Hadlock.
“I’ll be sharing tips, “tricks”, and experiences that have helped me through my medical journey. As many ostomates have done for me since my first conference in 2017, this year my goal is to help others feel welcome and have breakthroughs of their own,” Hadlock says.
Those active on social media may see some other familiar faces such as Kristen Furey, The Furey Fighter. “I’m excited to share my journey with Advocacy and what it has done for me in terms of growth and acceptance with an ostomy!” Furey says. “I am most looking forward to attending my first UOAA ostomy conference and being around so many other people who have similar health conditions and an ostomy! Knowing they have walked the same journey that I have and hearing from them firsthand their experiences with an ostomy!”


Speaking on Parenthood it will also be the first conference for Meghan Brown (@EMC_Brown) “I am most looking forward to meeting longtime ostomy friends and experiencing my very first conference, as well as hearing some of my closest ostomy friends speak!”
“For my talk, I’m excited to share more about my experiences of pregnancy with an ostomy and what life looks like now with a very curious three year old and wild 20 month old. I’ll shed a little light into the funny but important conversations I’ve had with my three year old about my ostomy, and how we maintain an open dialogue around all things ostomy.”
Molly Atwater-Pulisic will be joined with Collin Jarvis in leading many of the other topic discussions. Check out the full conference schedule. Young Adults between the ages of 18-25 get the special price of $135.00 for all three days.
Caregivers Track
Partners or caregivers of ostomates are also encouraged to attend UOAA’s National Conference this summer. Register and you’ll be welcomed for all the social events and food and drink opportunities and receive access to the informative Exhibit Hall.
Special sessions are also exclusive to caregivers on Friday August 11.
The Caregivers Track that morning will feature a Caring for a Male Rap Session and a Caring for a Female Rap Session.
An important session on Caregiver Stress – How to Cope will be available that morning a well.
Pediatric Track
The youngest of ostomates and their parents/caregivers will also have a special track at the conference.. This day-long program is held on Saturday and will be led by pediatric WOC Nurses and ostomy parents.

Some session highlights include:
Advice from an Ostomy Parent with Julie Hubbard
Dietary Considerations in GI/Ostomy Patient with Erika Kay, RDN, LD 9:15am to 10:30am Ask the Expert: Gastroenterology Care of the Pediatric IBD Patient with Dr. Allison Wyatt
Ask the Expert: Surgical Management of the Pediatric IBD Patient with Dr. Rueben Rodriquez
Ostomy Complications and Pouching Techniques with WOC Nurse Maryanne Lewis
Ask the WOC Nurses with Barbara Richardson, Erika Guidry and Sharon Wallace
Exercise and Activities for Children with Ostomies with Tenille and Rebekka Smith
Children between the ages of 5-17 are just $25 and the one-day rate for parents is $125.00
Volunteers from around the country are working hard to create a life-changing experience for the young ostomate community. Register by May 31st to get the early bird discount. Please spread the word, invite a friend and discover your people this August in Houston.





 saved her life. She also wants to serve as an inspiration to other young people facing similar challenges and let them know they can “live the life they want because of the ostomy bag” and not in spite of it. Sydney exemplifies the resilience of the ostomy community.
saved her life. She also wants to serve as an inspiration to other young people facing similar challenges and let them know they can “live the life they want because of the ostomy bag” and not in spite of it. Sydney exemplifies the resilience of the ostomy community.
 from wonderful WOC nurses, experienced ostomates, amazing doctors and dedicated advocates.
from wonderful WOC nurses, experienced ostomates, amazing doctors and dedicated advocates. The event will come to a close with a special presentation from Magen Cherry, a j-poucher and winner of the 2007 Miss Texas USA competition. She uses her platform to share encouragement and bring hope to fellow ostomates and j-pouchers coming to terms with their new reality. Fun fact: Magen had a colonoscopy three days after being crowned Miss Texas USA!
The event will come to a close with a special presentation from Magen Cherry, a j-poucher and winner of the 2007 Miss Texas USA competition. She uses her platform to share encouragement and bring hope to fellow ostomates and j-pouchers coming to terms with their new reality. Fun fact: Magen had a colonoscopy three days after being crowned Miss Texas USA!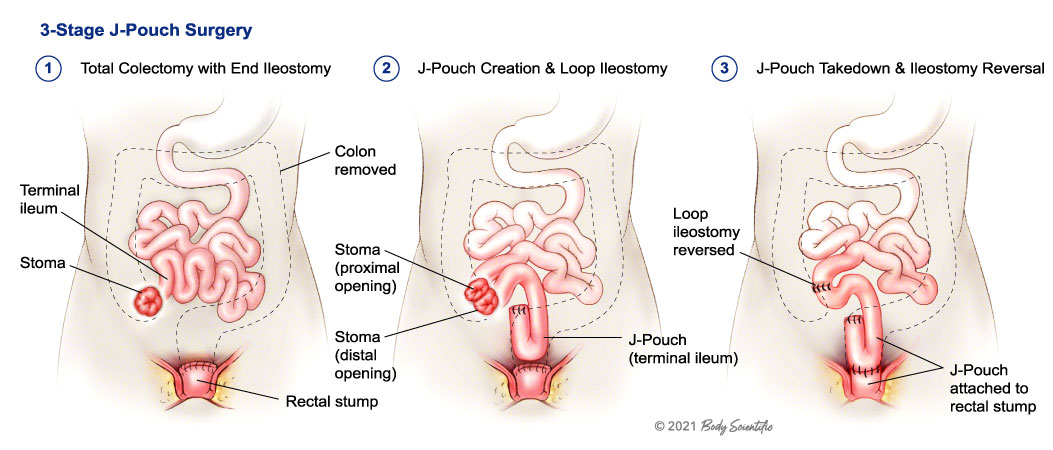
 another proud scar.
another proud scar.

