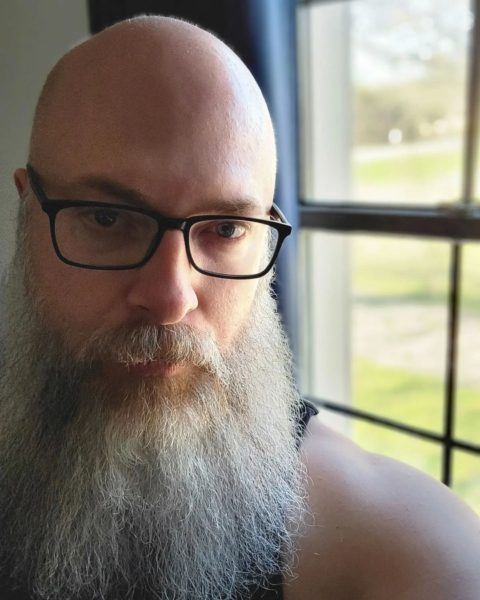
Micheal’s Urostomy Story
Bladder Cancer at Age 40 and the Path to Recovery
By Micheal Heath Waid
I noticed the faint pink color in my urine in November of 2018. I wasn’t sure what to make of it, but I mentioned it to my husband and he, being a nurse, suggested I see my General Practitioner immediately.
I made the appointment to see her. Assuming a UTI, she blamed me for “wearing dirty underwear” because it’s unusual for men to acquire that sort of infection. She tested me for an infection and gave me a prescription for antibiotics. Offended by her comments, I didn’t say much else. I took the medication and didn’t see the pink again. I assumed everything to be alright.
But then I saw pink urine reappear in August of 2019. I went back to my GP. Less snarky this time, she advanced a referral to the Urologist. The normal scans followed and discovered an anomaly in my bladder. A later cystoscopy confirmed two smallish tumors. The next parts of my journey are fairly standard. A Transurethral Resection of the Bladder Tumor followed the cystoscopy. The pathology from which confirmed muscle-invasive bladder cancer, Stage II.

Micheal with his husband James, a nurse, who encouraged him to see a doctor at the onset of his bladder cancer symptoms.
I had not heard many cancer survival stories. I spent a few days being completely devastated by the news, but fairly quickly something shifted me into business mode. I spoke with the Urologist who recommended chemotherapy followed by bladder removal. He explained the surgical options. He also explained that if I chose to not have the surgery that this cancer would ultimately result in my death.
Hearing that is not easy, but this decision was the easiest part of this entire experience. I elected to go through with the Radical Cystectomy to remove my bladder, prostate, seminal vesicles, and pelvic lymph nodes. I also elected, upon his recommendation, the neobladder option of urinary diversion. This Urologist would perform the surgery.
Port placement and chemotherapy next. Methotrexate, Vinblastin, Doxorubicin, and Cisplatin were the drug therapies the Oncologist felt would give me the best outcome. There were no illusions that chemotherapy would be the cure. Instead, they were used to increase my chances of survival post-surgery.
This Oncologist and the infusion nurses are the best medical professionals I have come across to date. The standard of care for chemotherapy recipients is off the charts here – which is wonderful because the chemotherapy portion of this trial is the worst experience I’ve ever endured. Trying to work through my chemotherapy proved much harder than I predicted, and I basically failed in that. I felt horribly sick all the time. I slept fourteen hours a day. By the end of my infusions, outside of the usual side effects of the drugs, I had developed several mental associations and the thought of certain mundane things made me feel sick. The thought of putting ice in my mouth made me sick. Receiving fluids to stave off dehydration made me sick. I could taste everything they injected into me. Luckily I only received four infusions, but I wouldn’t wish that on my worst enemy.
Surgery came about five weeks after chemotherapy ended. This gave me enough time to get some strength back. I still didn’t really have my hair back, but the beginning stages were sprouting.
This is where my fairly standard journey shifted. My surgery did not go as planned. I went under assuming I’d wake up with a neobladder, but instead I woke up with a urostomy.
My surgeon encountered complications in my abdomen that left him unable to create the neobladder. He consulted with my husband and they decided to go with our agreed-upon Plan B, the urostomy. The surgery took twice as long as planned, and according to my surgeon he was barely able to complete the urostomy because my blood vessels are “too short”. I’ve never thought of any part of my body as petite before.
I’m open about my circumstance and have realized that while bladder cancer is one of the most common cancers in the world, most people have no idea what this is all about
Post-surgery, I experienced a kind of reaction that cannot be fully explained. My kidneys were not functioning properly. My output was incredibly dark. So dark that they called in a Nephrologist for advice. My surgical team blames a drug called Toradol for the reaction while others blame the lengthened surgical process. I’m not really sure of the culprit but I am sure that I have permanent kidney damage from that surgery. The Nephrologist got me back on track quickly though.
This led to an extended stay in the hospital. Seven days total with intense back pain and lackluster care. I know that urostomies are not very common, but the nurses I encountered had very little exposure. One nurse throughout the week really knew how to apply the set up. It leaked a lot while in the hospital.
An ostomy nurse did visit me a little bit. I feared anyone touching my incision or my new stoma and couldn’t stop convulsing every time she tried to touch my abdomen. I know it frustrated her but it felt uncontrollable. She eventually quit coming by. They put us in touch with the major urostomy supply manufacturers so that we could begin ordering samples and from then we were on our own to figure out what worked. I haven’t seen an ostomy nurse since.
Recovery felt long. Six weeks away from work to heal. Moving was a challenge. Trying to sort out how to keep my urostomy from leaking challenged us. In the follow-up pathology from my surgery they also discovered that I had a second primary cancer in my prostate. Lucky to have had that removed as well.
It’s been a little over two years since my surgery and I’m doing well. I’ve sampled different supplies, and tried different ways to apply them, some successful and some not.
When I experience a leak I try to laugh about it. I am only 43 now with this permanent urostomy and I can’t spend the rest of my life being miserable. I choose to laugh when I pee on myself. Some times are harder than others, but overall I am pretty successful. I’m open about my circumstance and have realized that while bladder cancer is one of the most common cancers in the world, most people have no idea what this is all about. Luckily I’ve only encountered incredibly caring and receptive people.









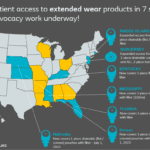 Coloplast 2022
Coloplast 2022
Thanks for sharing your story. Mine isn’t all that much different. It began about ten months ago with the same pale pink urine that was ignored since it went away. As in your case it came back.
Differences are that I’m 81 years old and about 5 months from my surgery.
As in your case I also had little help with learning how to manage my urostomy and had to figure it out myself. I’m also still struggling with some unexpected symptoms since the surgery.
Anyway… thanks again.
Steve Silberman
I have been through the same procedure. It was 2016 and I also struggled with leakage. I finally began using an Adapt Cera Ring which stopped any leakage. I use a 2piece skin flange and pouching system. Joining the UOAA has been wonderful. Local chapters are a lifesaver providing so much support.