By Tony Plonner
Editor’s Note: UOAA is proud to recognize Veterans and supports all those now living with an ostomy or continent diversion.
As a 20-year-old, way back in 1972, entering Army basic training was a daunting experience, the “fear of the unknown” had my mind reeling of what could happen. My approach was to take the challenge one day at a time, one hour at a time, or if necessary, one minute at a time.
We adopted many phrases to get us through the many challenges of this new environment: “Can Do!”, “When the going gets tough the tough get going” and when all else failed, “Yes Drill Sergeant!’ and we’d jump into the challenge at hand. This experience taught us we could surmount obstacles we’d never dreamed of. Unknowingly, our training prepared us for many of life’s challenges both in and out of the military. For me, progressions to Military Police School and Officer Candidate School strengthened my confidence and allowed me to take on challenges in both the military and civilian worlds.
One basic premise I learned was to never quit. I learned the quitter never knows how close they were to success. Whatever the challenge, you keep moving and keep fighting.
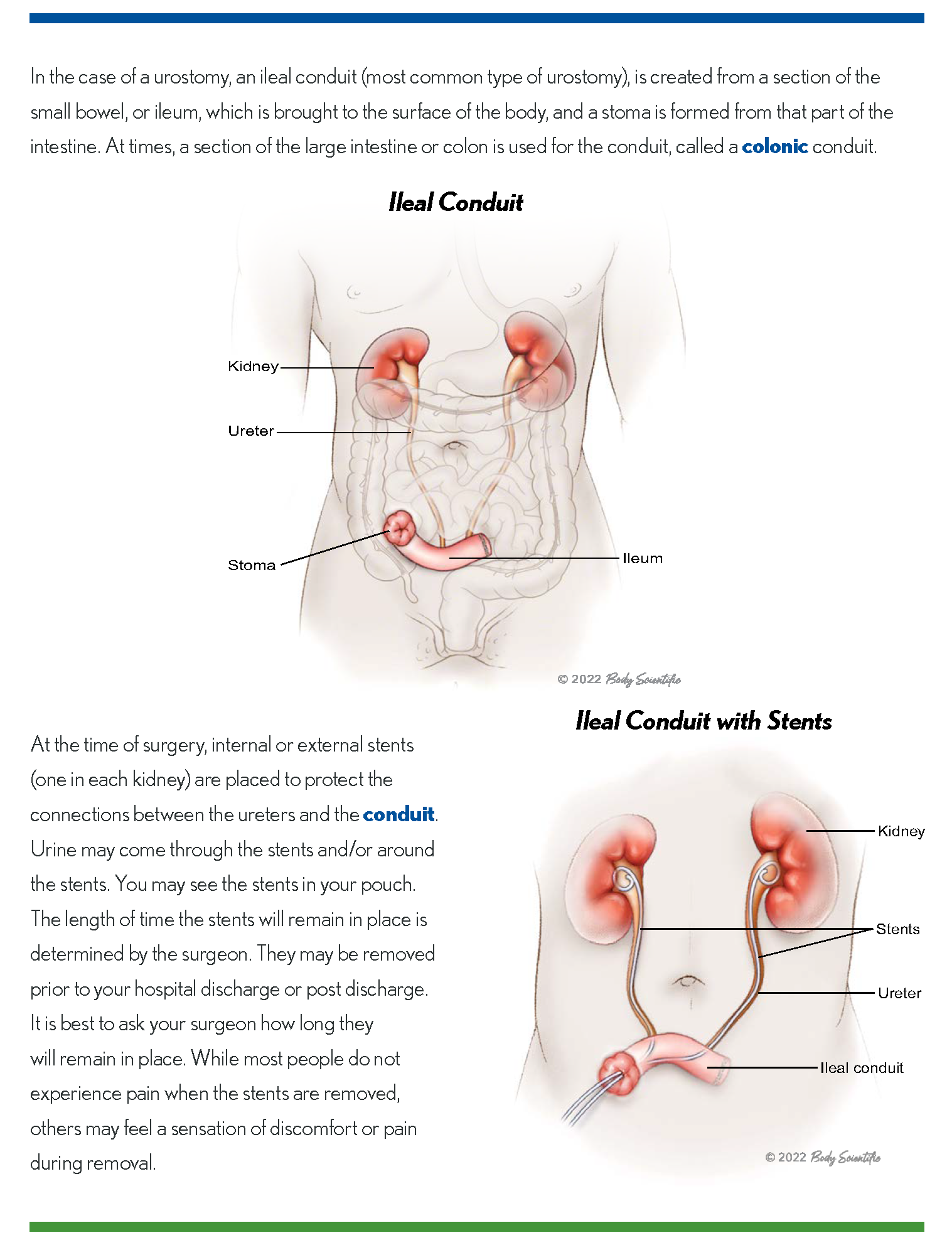
A little over thirty years ago, I was diagnosed with prostate cancer. Surgery and radiation followed. I kept a positive outlook and survived the experience. Unfortunately, a couple of years ago, I was diagnosed with bladder cancer. I was told there was a chance the radiation many years before may have led to this cancer. As it was muscle invasive, and with a history of radiation, all the doctors involved agreed the bladder would have to go. I had faith in my team and after a round of chemotherapy, I had urostomy surgery at the University of Miami Medical Center on March 14, 2022.
My best advice for those about to undergo or have recently had urostomy surgery for bladder cancer is to keep the “Can Do” attitude and continue with your life’s goals. You’ll be amazed how far you’ll go.
Having been told the result of the surgery would result in an ostomy, I researched as much as possible to learn about the side effects and the changes to my lifestyle I’d encounter. A pleasant result of this research was finding the tremendous support network available. I learned about the Bladder Cancer Advocacy Network (BCAN) and through my old army buddy, Justin Blum, United Ostomy Associations of America (UOAA).

Tony Plonner, pictured riding the Florida Keys Scenic Highway has continued an active lifestyle after urostomy surgery for bladder cancer.
Reading case stories, with a bit of skepticism I’ll admit, I learned of the many people who have not only survived but thrived through this experience. Along with my experience of tackling the unknown in the Army, and the great support of family and friends, these stories only bolstered my faith that we’d lick this cancer and continue with life.
My doctors regaled me with stories of ostomy patients maintaining their lifestyles, skydiving, running, golfing and barely missing a beat after surgery. Combined with the experiences of ostomates I’d read about, was confident I’d go through the surgery and, despite new limitations expected on my lifestyle, I’d take the hill and keep on moving.
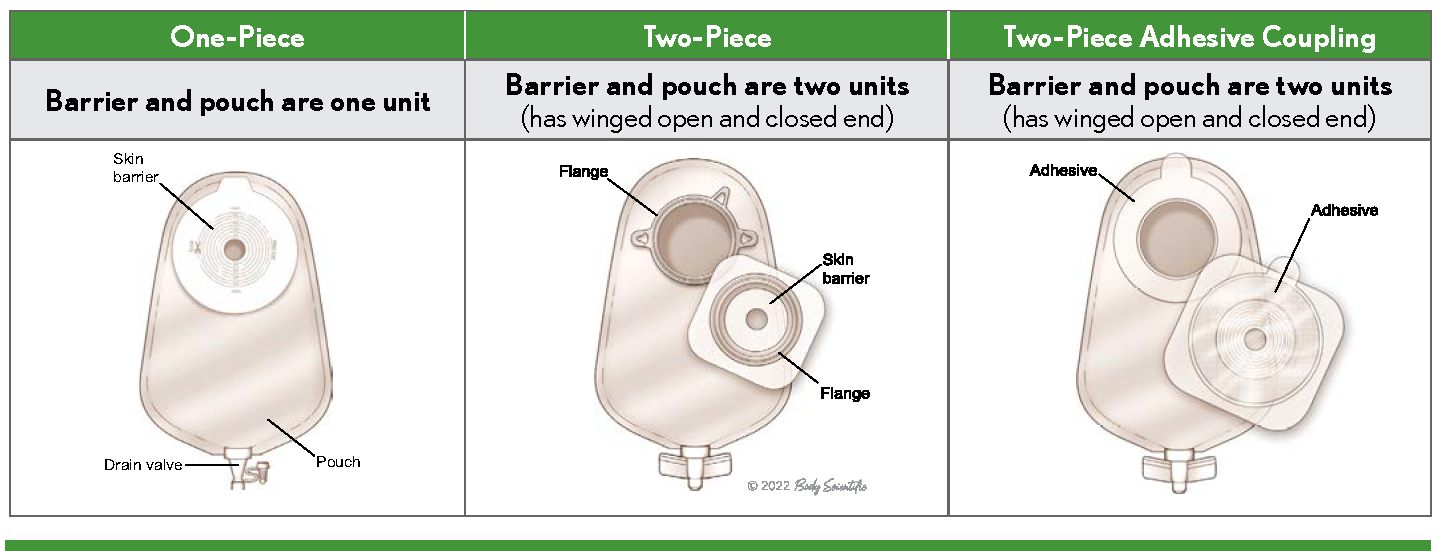
Looking back over the last year and a half I am astonished at how smooth, if that is the right word, the transition has been. Beginning with the support of the team at the surgery center, who trained me in the care of my ostomy, I followed orders like a good soldier, paid attention to their instruction and thankfully have made the transition to ostomate.
My biggest concerns, changes to my lifestyle, were pretty much unfounded. I am an avid golfer, road bicyclist, and generally an active person. I was concerned about how my ostomy bag would affect these pursuits. The answer is hardly. I wondered how I’d be able to go on bike rides of 15 or 20 miles in tight bike shorts and was pleasantly surprised to find it pretty comfortable. Also, it is easy to tell when I need to pull over and go to the bathroom. Spandex bike shorts don’t provide much wiggle room!
Golfing also has been unaffected by my ostomy. I was worried about the twisting during the golf swing and any stress it would put on my appliance. It hasn’t been an issue. Now, if I could only lower my handicap…
My best advice for those about to undergo or have recently had urostomy surgery for bladder cancer is to keep the “Can Do” attitude and continue with your life’s goals. You’ll be amazed how far you’ll go.





 events with partner organizations and others leading up to and immediately after World Ostomy Day. Follow us on
events with partner organizations and others leading up to and immediately after World Ostomy Day. Follow us on  So, what can I do now that I have a urostomy?
So, what can I do now that I have a urostomy? There are so many other things I have been able to do since my
There are so many other things I have been able to do since my 
