Bladder cancer and urostomy surgery do not stop Annemarie from living her best life.
I am a bag lady. I am highly educated and employed, yet carry a bag wherever I go. I don’t leave home without it. Because of bladder cancer, I have a urostomy. Like many other women, it took some time for my diagnosis. At 57, many of the symptoms I experienced were attributed to my age: menopause, UTIs, kidney stones, fibroids, etc. Thanks to the fibroids, I was scheduled for an ultrasound. It was my gynecologist who found the bladder tumor. She referred me to a urologist. In fact, she insisted. Her office called to make sure I followed through. I met that week with a local urologist. He did a scope. I saw him look at the nurse, concern written on both their faces. He started talking about surgery and apologizing for the diagnosis. In my naivete’, I had gone to the appointment by myself. I don’t remember him even saying the words, but I had bladder cancer.
Scans and a transurethral resection of a bladder tumor (TURBT) were scheduled for the following week. Usually an outpatient procedure, I was in the hospital for 4 days due to heavy bleeding after the TURBT. The tumor was large and the doctor couldn’t get it all but he thought it had penetrated the muscle. Unfortunately, the pathology was inconclusive so he did another TURBT the following week. The outcomes were exactly the same so we both decided my best chances were for a second opinion at Dana-Farber Cancer Institute in Boston. Throughout our discussions, he explained what my future might entail. It looked likely that they were going to have to remove the bladder and I would either have a new “bladder” or a bag. Quite honestly, I had no idea what it entailed, but I was horrified.
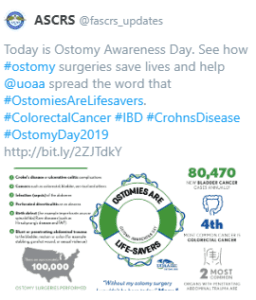
Dana-Farber is an amazing place. I had a whole team in place: a medical oncologist, an oncology urologist, a nephrologist, among others. The plan was an MRI to confirm the tumor’s pathology, a nephrostomy tube, chemotherapy and, if the cancer had not spread, a radical cystectomy. If it had spread, I would not need surgery but would be eligible for palliative care. Who would have thought surgery is the best case scenario. Due to claustrophobia, and despite anesthesia and Ativan, I moved so the MRI was inconclusive. I needed another TURBT. Thanks to my new amazing surgeon, the tumor was removed and the passage to my kidney was cleared. The pathology of the tumor showed no spread to the muscle and an ultrasound showed no more kidney hydronephrosis. Even better, I would no longer require chemotherapy. I did try immunotherapy with BCG but it did not work. The cancer was aggressive so we had to treat it aggressively. My radical cystectomy was scheduled for January 25, 2019.
It took me a long time to get there. I even asked what would happen if I did not receive the surgery. I would be dead in a year.
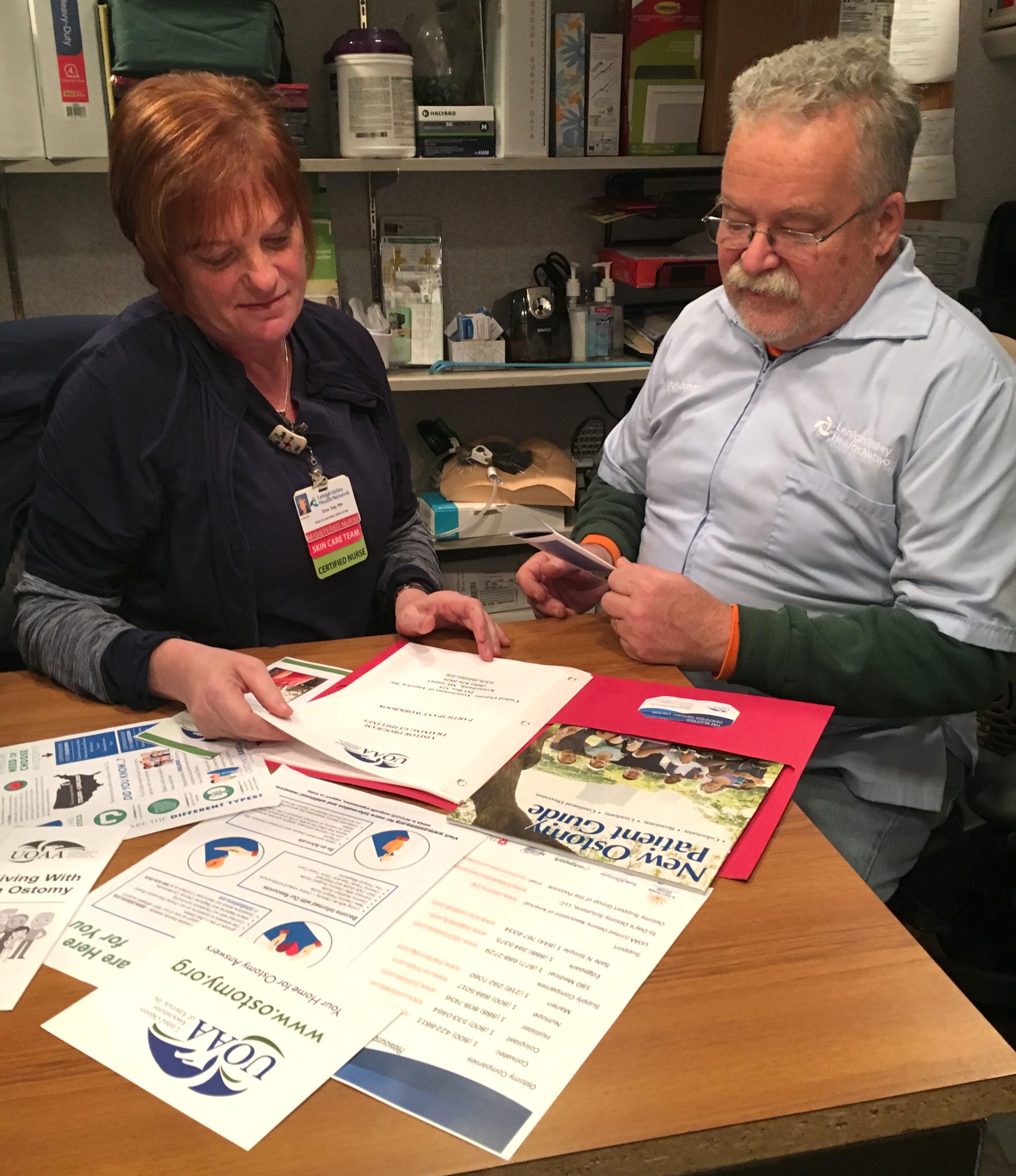
Wow, that was sobering. Because of the proximity of the tumor, I did not qualify for a neobladder. I would have to have a urostomy. Every time I talked about it, or even thought about it, I cried. I felt like I was going to be a freak. I offered my husband a divorce if he wanted one. I was devastated and frightened. I have learned that fear of the unknown and our imaginations are far worse than the reality. While so much of what had happened to me was out of my control, I did have control over one thing: HOW I handled everything. I decided knowledge was power. I was fortunate. My hospital had a class for urostomy candidates. For the first time, I was able to see an actual urostomy pouch. I was given hands-on instruction on how to change a bag. I met ostomy nurses (the best people in the world!) who would be helping me.
I decided I would be the one to handle my changes, right from the start. I would take control.
My surgery lasted 7 hours. I needed a transfusion but things went well otherwise. The surgery was not easy. People have described it as feeling like you were hit by a bus. I never really had any pain. It was easily managed with Tylenol. However, I was so weak. I eventually needed an iron transfusion. The one thing I wish I had gotten for my return home was a shower chair. Showers were the worst for me. It took me two months to feel more like myself and another month before I felt ready to return to work. I also cannot say enough about getting a good ostomy nurse. I have been described as a delicate flower (surprising to those who know me). I have very sensitive skin. The nurse was a Godsend to me in trying to manage all of my skin issues. After my visiting nurse visits ended, I continued to see the ostomy nurses at the hospital where I had my surgery. It took a year but, through trial and error, I finally have gotten a handle on things.
I had a few leaks. They were usually caused by user error. They were not the huge floods I expected. Honestly, none of this was as awful as I expected. So many people said this would be my “new normal”. I can’t stand that term. I call it my new reality. There isn’t anything normal about having a urostomy. However, it is very doable. I now wear two-piece bathing suits. I didn’t before. I am wearing the same clothes as I did before. I can kayak, hike, ride my bike, swim for hours, anything I did before. I was here for the birth of my first grandchild. I am back to work, a job that I love. I am not shy about talking about my bag to others. It is not a secret. In fact, I am kind of proud of it. I am alive and life is good.