By Ellyn Mantell
From the time I can remember, constipation was always an issue for me. I assumed I was doing something wrong to cause it. It turns out that I was born, like so many, with a redundant foot of bowel, which in layman’s terms, means that my colon was not only oversized, but a portion of it went in the wrong direction. Here is what I mean…the colon or large intestine ascends on the right side (ascending colon) and goes across the abdomen (the transverse colon) and descends the left side (the descending colon.) That is exactly the path that stool takes in its journey to leave the body. My redundant foot of bowel meant that the transverse colon actually went up at the connection to the descending colon, for a foot, before heading downward, so stool had to travel against gravity before leaving my body.
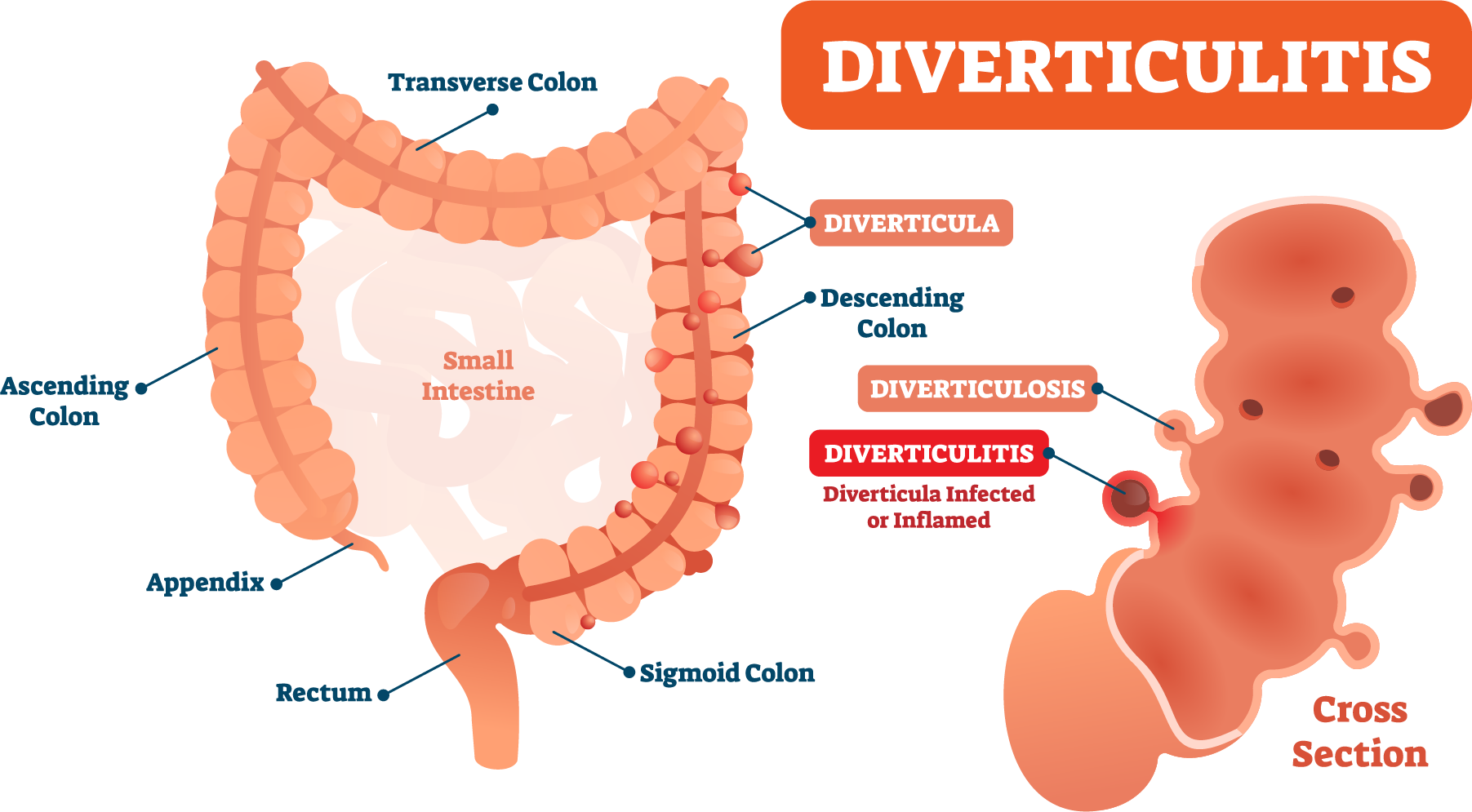
My first barium enema was when I was 10 years-old, and although we didn’t know what the problem was, I was always told at that time, and every subsequent test, that my sluggish bowel would be an issue for me, (and it truly was, until my ileostomy 6 years ago). So, it came as no surprise that I was also told, each colonoscopy or c-t scan, that I had severe diverticulosis, which could become diverticulitis, a problem that often requires medical intervention.
The diverticula are small sacs that form along the mucosal lining of the colon, often due to straining to move stool through the intestinal tract, which puts pressure on the intestinal wall (which causes the bulging). This issue can worsen with age, medications and other causes of constipation. If the diverticula are inflamed or rupture, serious infection can result, which then is called diverticulitis.
While diverticulosis doesn’t cause discomfort, diverticulitis can be terribly painful, cause fever, constipation or diarrhea, nausea and fatigue. Several in our Ostomy Support Group have had resections of their colon and ostomies due to diverticulitis. Some choose to be reversed after the several weeks of healing necessary to allow the connection in the intestine to do its job. Others choose, instead, to live with their ostomy, which offers them freedom from constipation.
There are ways to avoid diverticulitis, and they are manageable for most. Eating a high-fiber diet rich with fruits and vegetables and whole grains is a great place to start. You may remember that I have also mentioned that is a smart way to enhance our immune system, which may help fight Covid-19. Add more fluids, and if possible, pitted watermelon, for an extra kick of fluid. These tips will soften waste and help it pass more quickly through your colon. That may reduce the risk of diverticula becoming inflamed. Also, exercise and maintaining a healthy weight are very helpful.
Many physicians recommend reducing red meat; some used to say avoid nuts and seeds, although that restriction seems to have changed. As I tell others with an ostomy especially those with an ileostomy, if you eat nuts and seeds and fresh fruits and vegetables, which are healthy and filling, please chew, chew, chew, since that is the best way to avoid inflammation or a blockage.
Many medications can impact motility of the bowels, so be mindful to changes when you add or delete medications, and please address with your physician any concerns. And most important, if you notice any changes, pain, distention, nausea, vomiting or generalized discomfort in your abdomen that has you concerned, do not wait. Speak with your physician and consult UOAA’s blockage card and don’t be hesitant to go to the Emergency Room if needed. Much can be done to not only make you feel better, but to prevent a manageable situation from becoming extremely serious!
Ellyn Mantell is a UOAA advocate and Affiliated Support Group leader from New Jersey. You can follow her personal blog at morethanmyostomy


