Good News for Ostomates with Medicaid in Some States
By Jeanine Gleba, UOAA Advocacy Manager
Too many people living with an ostomy have the worry that due to a need for frequent pouch changes or a high output stoma they will run out of their monthly Medicaid allowable ostomy supplies. For the past year, UOAA has been supporting efforts, led by Coloplast, to expand Medicaid coverage of extended wear products in states with remaining access problems across the country.
UOAA’s advocacy work has included:
- Raising awareness on this important issue
- Recruiting Affiliated Support Group leaders that are also WOC nurses and other local clinicians to provide clinical support and insight
- Sending letters to state divisions of Medicaid services urging them to review the ostomy supply policy regarding coverage of ostomy supplies for HCPCS codes and quantities, specifically for extended wear products.
As the voice and leading organization advocating for people living with an ostomy, we know first-hand how important access to ostomy supplies are for our patient population. We share the patient perspective with testimonials from advocates as well as explaining patients’ unique needs, such as those who are unable to achieve normal wear time with a standard barrier. Improved access to extended wear barriers will assist those who do not have an optimal fit or have a high-output stoma and go through more standard wear barriers and pouch changes. For these individuals extended wear products would be the prescribed solution.
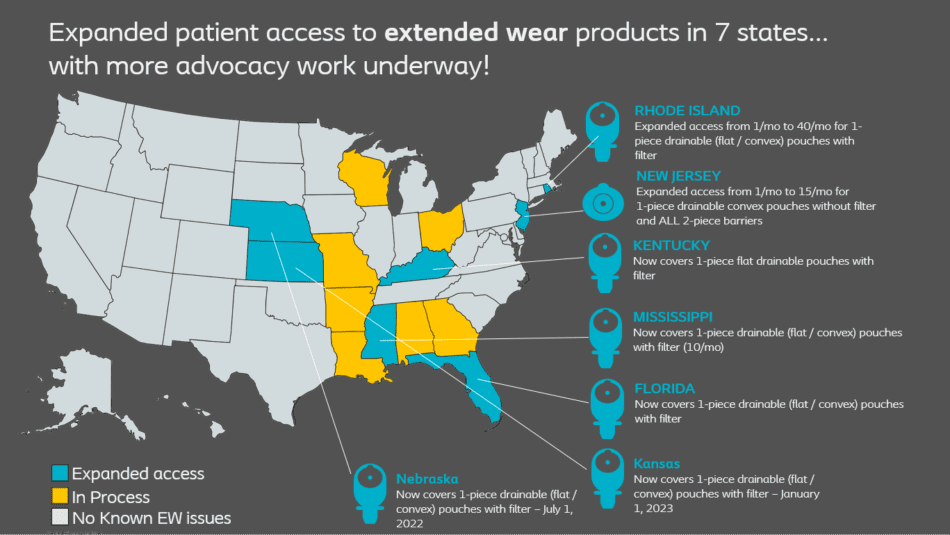
As a result of the collaboration between Coloplast, UOAA, State Home Medical Equipment (HME)/Durable Medical Equipment (DME) Associations, local clinicians and other advocates, we have expanded patient access to extended wear products in seven states as noted in the above map. This is excellent news for Medicaid beneficiaries living with an ostomy in these states! (Note: States that are grey/light blue on the map were not seen to have any state Medicaid extended wear access challenges.)
More advocacy efforts are underway in Alabama, Arkansas, Georgia, Louisiana, Maryland, Missouri, Ohio, and Wisconsin to remove the current barrier to access in those states. These states have Medicaid coverage that is much less than the current Medicare standards.

 Coloplast 2022
Coloplast 2022








I am a Family Nurse Practitioner and have an ostomy. I would love to provide services in my rural community to ostomy patients. There is nothing to help them really. I don’t know where to start.
I just wanted to say thank you for what you are doing for us ostomates 😊
Is a colostomy reversal is covered by Medicaid?
Generally, surgical procedures are covered by Medicaid as long as the surgery is ordered by a Medicaid-approved physician and is deemed medically necessary and is performed at a Medicaid-approved facility. Specific eligibility criteria and reimbursement amounts vary in each state. Find Medicaid contact info for your state at https://www.medicaid.gov/about-us/beneficiary-resources/index.html
Hi I live in north Georgia and have Medicaid connected to my ssi currently for disability. I don’t not qualify work credits wise for SSDI unfortunately or Medicare since I’ve been on SSI – Disability for 3 years now. So georgia Medicaid is what covers my supplies for ostomy bag except for a huge part of those expenses which are the actual BAGS themselves. They cover all the supplies wipes and related powder and barriers to put and keep the bag on for a few days but my bags aren’t covered at all under georgia state Medicare due to the fact that they are “High output” insurance code – which is absolutely medically necessary for the type of high output ileostomy I suffer from. I only have a bit less than 3 ft of remaining bowel and no large bowel or colon remaining at all.
My doctor wrote letters of medical necessity about this to my ga Medicaid insurance but they replied that the rule not to cover high output supplies was set in stone and no exceptions can be made for medical necessity. So I have to pay $85-$175 a month depending on how fast my bags leak and need replacing as an expense due to my medical problem and it is very necessary to always have a secure bag on! Interested if ANY other states Medicaid DOES cover high output ostomy bags? It might just be worth the move.
Georgia also provides $0.00 state supplemental income to the federal ssi amount (currently $914.00) that all states get. I know California provides something like 199$ and change state supplemental income to the federal amount currently of $914.00. To all with disabilities not just elderly and or blind like nevada. I know some states may provide more in amount of state supplemental income to the federal ssi as well. Anyone happen to know more about which states and what strings if any are attached? I’m very interested in a state Medicaid I would
Qualify for as a ssi disability recipient that covers high output code ostomy bags plus the needed supplies (barrier wipes, bag barriers since they’re a two piece system, in addition to the bags and adhesive remover wipes, zinc powder, extra strips of adhesive to go around the bag to prevent leaks, rings, etc. basic ostomy supplies needed for a bag change. I can rule out Alabama which I have heard that the Medicaid there doesn’t cover ANY ostomy related supplies, which sounds like hell on earth to me, yikes! Thanks!