Are you a new ostomate? Or a soon-to-be ostomate? No matter how far you are in your ostomy journey, adapting to your new situation is an inevitable part of the process. Talking to others who have already been in your shoes can help you in adjusting to this time of your life. That’s why we asked Josh Nelson, the first active-duty U.S. Airforce Pilot living with an ileostomy, to share his story and his experience with his ostomy journey to give insights on how getting an ostomy can be just the beginning of an exciting new chapter.
Before surgery
What was your life like before your ostomy surgery?
I was diagnosed with ulcerative colitis in November of 2017. Throughout the next year after my diagnosis, I tried maximum medical therapies starting with oral medications, then biologics, and then transitioned to combination therapies with biologics. Unfortunately, my body just did not respond to the medications, and the disease just took over my life. If you want to talk about quality of life with ulcerative colitis before I had the surgery – I didn’t have one. I was 145lbs. I was having 18 to 20 bowel movements a day. I wouldn’t leave my house. I knew where every bathroom, rest stop, and gas station were from my house to where I work. Any time I did leave the house, the only thing on my mind was, “Where’s the bathroom?” in case I had that sudden urgency to go. My wife and daughters left me alone. They wouldn’t even ask if I would go with them anywhere because they just knew I did not want to go anywhere. I had no quality of life. I was a prisoner in my own home, and that’s no way to live your life.
How did you feel when you learned you would be having ostomy surgery? What questions of fears did you have?
I made the decision to have an ostomy surgery in November of 2018, and I had about three days’ notice before the surgery was going to take place. The staff at the University of Minnesota Medical Center, where I was inpatient for 30 days prior to surgery, did a great job of introducing what life with a stoma will be like. My questions were, “What is a stoma?” “What are the appliances that I’m going to have?” “How do I care for this thing, and how do I recover?” and “How do I slowly adapt to having an ileostomy and then getting my life back?” The WOC nurses were great, because they would just simply start to explain, “Oh, here’s what a wafer or barrier looks like,” “Here’s what a pouch looks like,” “Here’s what some of the accessories are.” They also explained, whether it’s ileostomy, colostomy, or urostomy, people do go on to live fully functional lives.
I definitely had some goals, but I had no fears when it came to having the surgery. I mean, okay, fine – I had maybe a couple fears of having surgery, but the stoma itself I was not afraid of. The reason for that is because I was kind of at my lowest of lows, and I thought to myself, “How could this be any worse than what I’m dealing with right now?” I remember my surgeon and the medical staff told me that once the surgery was done, I would no longer have the pain, and each day moving forward I could start to focus on getting my life back.
What advice do you have for people who are considering ostomy surgery?
My advice to anybody who is considering having the surgery is to keep an open mind. It will take some work. You will need to adapt to what you have. That means taking care of yourself physically, mentally, and emotionally because it is a step-by-step process. It is a big transition, but I’ve done everything I could to make sure my quality of life has improved. I do not regret my decision one bit. I have my life back and that’s what I think is most important.
Coming home
What was your experience like right after your ostomy surgery?
I had about five days in the hospital after surgery, and during that time I was focused on recovery, protecting my abdomen, and getting my strength back. The nurses did a great job of explaining step by step what it takes to change out the pouch and care for my stoma. Before I left the hospital, I needed to make sure that my pain was under control, starting to move around, and understood how to change my appliance by myself.
What were your goals after your surgery?
I focused on transitioning to home life again, figuring out how to slowly heal my body, and how to start eating foods again.
My goals were:
- Getting healthy food into my body so that my body can recover.
- Finding out what schedule I should be on for changing out my appliance.
- Observing my stoma area regularly to keep my skin healthy, prevent skin breakdown, and make sure that my stoma was healing properly.
What would you tell someone else returning home from their surgery?
- Don’t be afraid of touching the stoma because your stoma doesn’t have any nerve endings you can feel.
- It’s extremely important to have a solid understanding of how to change your pouch and ask for products before you leave the hospital.
- Your WOC nurse will probably explain that what works best for you in the hospital may change after you go home and are healing up. Initially, it might be multiple times a week that you’re changing your whole appliance out because your abdominal area might’ve been swollen from the surgery, and as it starts to reside some of those wafers might fit differently.
- Everybody’s different. Everybody responds to products differently. Those first couple of weeks to a month is just trial and error to find out which products work best for you. After you figure out your change routine, your quality of life can start to improve. You no longer need to worry about having multiple leaks or having multiple issues with your appliance, and you can start to focus on making other goals for your life with an ostomy.
- Just take it day by day. Don’t think of the end state right away because it’s going to take time to get there. Create small goals on a day-to-day basis and then think long term and how to get there. It’s definitely a marathon; it is not a sprint. You’re going to learn something new every single day until you get comfortable living your life and understanding how to handle your ostomy.
Managing life with an ostomy
How has your life changed now that you have an ostomy?
I’ve had my ileostomy for over three years, and I can honestly say I haven’t looked back or had any regrets whatsoever to surgically remove my colon. I try to tell people my worst day as an ileostomate far exceeds my best day ever living under the umbrella of Inflammatory Bowel Disease. I am no longer bound by any type of medication. I have no special diet, nor do I have any restrictions, and my quality of life is through the roof. I could not be happier, and I do not regret the decision one bit whatsoever. But how did I get there?
 First off, I accepted the fact early on that I was going to have an ileostomy for the rest of my life because it was a decision I made for a better quality of life. After accepting it, I could focus on moving forward versus dwelling on the “how’s” and “why’s” with ulcerative colitis.
First off, I accepted the fact early on that I was going to have an ileostomy for the rest of my life because it was a decision I made for a better quality of life. After accepting it, I could focus on moving forward versus dwelling on the “how’s” and “why’s” with ulcerative colitis.
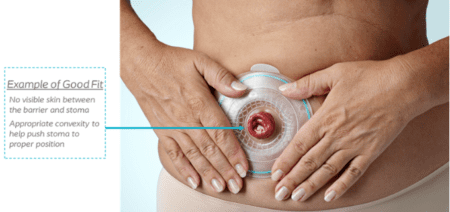
Secondly, after trying multiple different products, I came across a Coloplast product that worked really well for me. Once I found the product that worked well for me, that gave me the confidence to continue moving forward with my life and not have to worry about having leakage or skin issues. I have a couple routines, I’ll change my pouch no more than twice a week, but no less than once a week. I observe how the wear and tear of my wafer and appliance is working.
On top of that, I wanted to do everything that I could to make sure that I am living the best life that I can. I made some personal decisions, such as eating better and taking care of myself. I exercise quite a bit, and I try to eat fairly well. I try to focus on eating healthy foods so I can get the nutrition that my body needs.
What are some other tips you want to share about managing life with an ostomy?
It’s important to understand that this affects everybody differently, and it’s up to you to determine what works best for you to adapt, overcome, and live your life with any type of ostomy. I reached out to local support groups, and I think that’s extremely beneficial because you get connected with like-minded individuals. No matter whether they have a colostomy, ileostomy or urostomy, you can touch base with them and share your fears and concerns. A lot of these people have lived decades with their ostomy, and they’re proof to you that you probably can too. Finding that help and resource is extremely beneficial in helping you understand how to navigate life now that you have an ostomy and what’s out there for you.

I hope this helped you to understand what it was like to be diagnosed with the disease, have a permanent ileostomy, and how I live my life moving forward. Thank you! -Josh
*Josh has received compensation from Coloplast to provide this information. Each person’s situation is unique, so your experience may not be the same. Talk to your healthcare professional about which product might be right for you.

At Coloplast, we strive to provide innovative solutions to support people with intimate healthcare needs and make their lives easier. Now, we’ve got an app for that!
If you’re looking for additional support during your ostomy journey, download MyOstomyLife by Coloplast® Care. The app is designed to help you be successful and build confidence in managing your ostomy by providing you with personalized tools and resources for your daily life with an ostomy.
With MyOstomyLife, you can create a digital stoma journal to track your pouching changes over time and easily download to share with your nurse, if requested. The app also provides you with educational resources offering reliable product and lifestyle advice, tips customized to your ostomy type, and inspirational videos from other ostomates like Josh.
You can also easily contact one of our Coloplast Care® Ostomy Advisors for product and lifestyle support within the app. We’re here to help!
Download MyOstomyLife for free on your smartphone or tablet today to get started!
Have any questions about the app? Visit Coloplast® Care at www.ostomy.coloplastcare.us or call
1-877-858-2656.
Information provided in the app and from Coloplast® Care is for educational purposes only. It is not intended to substitute for professional medical advice and should not be interpreted to contain treatment recommendations. You should rely on the healthcare professional who knows your individual history for personal medical advice and diagnosis.
Editor’s note: This article is from one of our digital sponsors, Coloplast. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.


 First off, I accepted the fact early on that I was going to have an ileostomy for the rest of my life because it was a decision I made for a better quality of life. After accepting it, I could focus on moving forward versus dwelling on the “how’s” and “why’s” with ulcerative colitis.
First off, I accepted the fact early on that I was going to have an ileostomy for the rest of my life because it was a decision I made for a better quality of life. After accepting it, I could focus on moving forward versus dwelling on the “how’s” and “why’s” with ulcerative colitis.

 Mackenzie Bauhs, CWOCN, is currently an employee and Ostomy Clinical Consultant for Coloplast. She obtained her bachelor’s degree at Carroll University in Wisconsin. She has worked with ostomy patients in the post-operative period at the University of Wisconsin Hospital and Clinics in Madison, Wisconsin as well as outpatient ostomy care at Rush University Medical Center in Chicago, Illinois.
Mackenzie Bauhs, CWOCN, is currently an employee and Ostomy Clinical Consultant for Coloplast. She obtained her bachelor’s degree at Carroll University in Wisconsin. She has worked with ostomy patients in the post-operative period at the University of Wisconsin Hospital and Clinics in Madison, Wisconsin as well as outpatient ostomy care at Rush University Medical Center in Chicago, Illinois. enjoying a highly active lifestyle. So when I found out that I needed a stoma revision, I knew that my recovery would look very different from my previous surgeries. I knew that in order to improve my recovery time, decrease my risk for complications, and get back to the mountains, I had to put in more work.
enjoying a highly active lifestyle. So when I found out that I needed a stoma revision, I knew that my recovery would look very different from my previous surgeries. I knew that in order to improve my recovery time, decrease my risk for complications, and get back to the mountains, I had to put in more work. As you start your journey to recovery, you’ll experience that life after ostomy surgery is a new reality. No matter how far after surgery you are, you will need to adapt to your condition and cope with your new situation. If you’re looking for additional support during your ostomy journey, consider enrolling in Coloplast’s free online support program, Coloplast® Care! It is a personal product support program designed in collaboration with nurses to provide you with individualized product support and lifestyle education, and product access coordination. Coloplast Care is available when you need it – whether it is through our online educational resources offering reliable product and lifestyle advice, news and tips customized for your situation, or over the phone with our team of dedicated Ostomy Advisors. We’re here to help!
As you start your journey to recovery, you’ll experience that life after ostomy surgery is a new reality. No matter how far after surgery you are, you will need to adapt to your condition and cope with your new situation. If you’re looking for additional support during your ostomy journey, consider enrolling in Coloplast’s free online support program, Coloplast® Care! It is a personal product support program designed in collaboration with nurses to provide you with individualized product support and lifestyle education, and product access coordination. Coloplast Care is available when you need it – whether it is through our online educational resources offering reliable product and lifestyle advice, news and tips customized for your situation, or over the phone with our team of dedicated Ostomy Advisors. We’re here to help!


