There are two main types of stomas, and they both have certain “ideal” characteristics in common. Do you know what they are?
Wound care nurses know that it’s not uncommon to hear the terms ostomy and stoma used interchangeably, even though they have different meanings.
What is a stoma?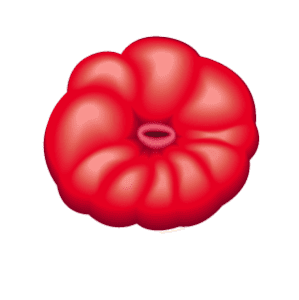
Let’s start with the basics:
- The stoma is the mouth-like, visible part of an ostomy.
- A fecal or urinary stoma is composed of mucous membrane or the lining of the intestine that’s exposed to the surface.
- Following ostomy surgery, effluent (output) — such as fecal matter, urine, or mucous — will pass through the opening of the stoma, called the lumen.
- The patient will not have voluntary control of the effluent expelled by the stoma.
Types of stomas
There two major categories of stomas: the end and the loop.
End stoma
An end stoma is created when the surgeon brings one end of the GI tract through the abdominal wall, then folds it over. The surgeon then removes the other end or sews it shut.
In some cases, the surgeon will create end stomas from both ends of the GI tract, called a double-barrel stoma. In this case, you’ll see two distinct stomas: the proximal stoma discharges stool and the distal stoma discharges mucous. Sometimes an expanse of skin separates the two stomas, and sometimes they will share the same opening. This construction is most common for infants or very small children.
Loop stoma
To create this type of colostomy, the surgeon lifts a loop of the transverse colon through the abdomen. The colon is given a small split on the side facing out, and a rod is placed underneath for support. The rod may be removed after a few days when support is no longer needed. The proximal opening of the stoma drains stool from the intestine, while the distal opening of the stoma drains mucus. Loop stomas are usually created for temporary ostomies.
Characteristics of an ideal healthy stoma
Each stoma is unique, just as each patient’s physiology is unique. Different surgical techniques will result in stomas of different appearance. At the same time, the “ideal” stoma has some identifiable characteristics:
Moist
The inner surface of the stoma continually produces mucus to cleanse the stoma. Mucus production is a normal function of the intestines that serves as natural lubrication for food passing through the body. The mucus gives the healthy stoma a wet appearance.
Beefy red
Blood flow is essential to the health of the stoma. Normal stoma tissue is highly vascular and will appear deep pink to red. Pale pink is also normal in a urinary stoma. Stoma tissue may even bleed slightly when rubbed or irritated, which is normal. When a stoma turns pale, or dark, it means there’s a problem with the blood supply, so be sure to investigate.
Round
A round stoma is easiest to measure with circular rulers. It also works best with pre-cut skin barriers (the part of the ostomy appliance that affixes to the skin and attaches to pouch). An oval or irregularly shaped stoma may require cut-to-fit skin barriers.
The shape is affected by the type of ostomy and the individual’s body composition. The shape can also vary with the wave-like muscular contractions of the intestines, the peristaltic movement.
Budded/protruding
When a stoma has a rosebud shape (rather than flat or retracted), it protrudes into the pouching system. This allows the effluent to fall out into the pouch away from the body. The ideal protrusion is 2-3 cm with a lumen in the very center.
Strategically located
To easily accommodate the skin barrier, it’s ideal to have 2-3 inches of flat skin around the stoma. Avoid beltlines, bony prominences, skin folds, suture lines, or the umbilicus (belly button). Also, the patient will have more success managing a stoma located in an area that they can see and reach.
Stoma assessment
The stoma itself has no sensory nerve endings, which means there is no sensation for the patient. In other words, the patient may not feel pain or discomfort if the stoma becomes lacerated or injured. Therefore, your thorough clinical assessment of the stoma and the surrounding skin is essential to catching problems early.
Ostomy basics for healthcare clinicians: upcoming wound care conference session
As the third largest wound care conference in the nation, Wild on Wounds (WOW) is focused on advancing the healthcare workforce with impactful, innovative, hands-on wound care education built by and for clinicians.
This year, Joy Hooper, RN, BSN, CWOCN, OMS, WCC, AWCC, will present, “Ostomy: Basics and Beyond” which will provide a better level of understanding of colostomy, ileostomy, and urostomy surgery. The surgeries will be explained in a simple, relatable show-and-tell progression that builds on healthcare clinicians’ understanding GI tract anatomy. The presentation will include the concepts of peristomal skin protection from output and the different types of appliances available. The session will also include trouble shooting common peristomal skin common complications.
The session is intended for dieticians, nurses, and physical therapists and offers 4.00 contact hours. Learning objectives from the session include:
- Identifying how to communicate basic ostomy care based on individual type of ostomy as it relates to a patient’s ostomy type
- Selecting interventions to preserve peristomal skin integrity
- Recognizing how to use ostomy products to customize fit thus promoting quality of life
WOW details
This year’s 17th annual WOW event is brought to you by the Wound Care Education Institute (WCEI) and Nurse.com, part of the parent company Relias’ family of brands. The conference will take place from September 13–16 in Hollywood, Florida. Conference attendees can choose from dozens of educational sessions and earn up to 25 contact hours for CE credits.
WOW offers innovative, interactive, and informative sessions, including simulation workshops, live product demonstrations, and a new pre-conference track with an entire day of legal sessions. Also new this year is a virtual poster hall featuring the latest in clinical research, clinical practice outcomes, evidence-based interventions, new technology, management of complex wounds, and more.
To learn more and register for Wild on Wounds, visit here.
-Natalie Vaughn, MBA, Senior Content Marketing Manager, Relias

 Exercising with an Ostomy
Exercising with an Ostomy Some people wonder how they can ever find something positive in something so scary as an ostomy, but it can be done. You don’t need to do it in big
Some people wonder how they can ever find something positive in something so scary as an ostomy, but it can be done. You don’t need to do it in big 
 Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary
Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary 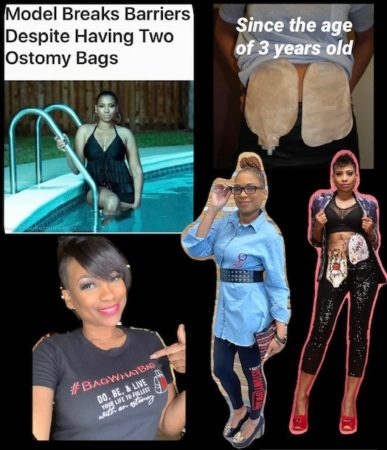







 search around the house and can’t find a sock or a bag worth using.
search around the house and can’t find a sock or a bag worth using. shining, a distant mountain range framed their joy – the chilly Alaskan rain held off.
shining, a distant mountain range framed their joy – the chilly Alaskan rain held off.
 Caregiving has been a consistent part of Taylor and Michael’s relationship. “When Michael had to have revision surgery, I wanted to make sure he’d have easily accessible food so he could focus on healing. I came over to his house prior to surgery and we made a few different meals to freeze. It was a great feeling for me that we got to spend time together cooking and his food would be taken care of while he recovered. He was used to taking care of himself so it meant a lot to me to do this for him.”
Caregiving has been a consistent part of Taylor and Michael’s relationship. “When Michael had to have revision surgery, I wanted to make sure he’d have easily accessible food so he could focus on healing. I came over to his house prior to surgery and we made a few different meals to freeze. It was a great feeling for me that we got to spend time together cooking and his food would be taken care of while he recovered. He was used to taking care of himself so it meant a lot to me to do this for him.” Even with partner support, Taylor says “UOAA has been so incredibly important to me in my ostomy journey. When I first got my ostomy, I scoured the UOAA website and read every piece of information I could find which helped ease my mind and answer my questions. UOAA’s website also helped me to be able to share information about my ostomy with family and friends.”
Even with partner support, Taylor says “UOAA has been so incredibly important to me in my ostomy journey. When I first got my ostomy, I scoured the UOAA website and read every piece of information I could find which helped ease my mind and answer my questions. UOAA’s website also helped me to be able to share information about my ostomy with family and friends.”