For most of my life, I measured the time it would take me to make it safely to the bathroom. If the bathroom dash was an Olympic event, I’d have won a gold medal! I often use humor when I talk about my condition, short bowel syndrome (SBS). But my story is one of hope, and how staying hopeful has helped me through each day. Of course, it was more than that. Living with a serious and chronic gastrointestinal disorder like SBS can require determination, persistence, and yes, even a sense of humor. I’m thankful I’ve had one my whole life. My name is Denise and this is my story.
| If you are living with Short Bowel Syndrome and rely on parenteral support, there’s an SBS Mentor available to connect with you. Click here to learn more. |
My Story Begins
As a teenager, I had an ongoing argument with my brother and sisters. Whenever it was time to do the dishes, I had to use the bathroom. They never realized that the reason that I had to use the bathroom every time we were done eating was because I had a medical issue. They just noticed that when it was my turn to do dishes I always disappeared. Nobody knew what was happening. In our family, we never went to the doctor and you put up with whatever you had going on. My dad and I were always racing each other to the bathroom to see who could get there first. I realize now that my father probably had some form of bowel disease, but he never was diagnosed.
When I was 18, I was diagnosed with Crohn’s disease. But I was determined to never let it get in my way. I got married and had three beautiful daughters. Along the way, I took a job as a 9-1-1 operator and eventually entered the police academy and became a police officer. Unfortunately, my first marriage didn’t last, but in time I met, fell in love with and eventually married a man who was then a member of the SWAT team. At that time, I finally felt like my life was falling into place—except for my recurrent Crohn’s flare-ups. Over the years, I had several surgeries caused by bowel obstructions. Each occurrence sent my determination into overtime. I wasn’t going to let anything stop me. I powered through each occurrence hoping it would be my last.
Then in 2009, even my unflappable hope and determination were tested after I retired from the police department. In November of that year, my husband developed a tumor on his spine, which left him paralyzed from the chest down. During this time, I cared for him and didn’t think about my Crohn’s disease at all. Although I didn’t want to admit it, the stress of caring for my husband around the clock took its toll on me. My Crohn’s disease got my attention like a house of bricks falling on top of me and one after another, complications set in.
Setbacks, Sepsis and Surgery
My daughter and her spouse moved in to help take care of my husband. Eventually I was hospitalized with yet another obstruction. Each time that I thought I was getting better, I’d suffer another setback. I became septic and had to go back to the hospital. I had an ileostomy to give my intestines and bowels a rest. If you are not familiar with an ileostomy, it is a surgically created opening in the abdomen in which a piece of the ileum (lowest part of the small intestine) is brought outside the abdominal wall. A stoma is created through which digested food passes into an external pouching system.
I was in the hospital for weeks, but I continued to worsen. I had horrible diarrhea and my electrolytes were off. Then I began having heart problems and was placed in the intensive care unit (ICU), where my kidneys began to fail. My body began shutting down and I was transferred to a specialty clinic. I was there for a month.
When I was finally discharged, I couldn’t leave the house for fear of having an accident if the ileostomy bag became too full and leaked—which it frequently did! After my surgery, food was moving too rapidly from my stomach to small intestines, an issue known as “dumping syndrome” – which caused me to experience a high volume of diarrhea. I had trouble keeping a good seal on my stoma site. Because of this, the skin surrounding my stoma became raw and infected. It was a vicious cycle!
My Diagnosis: Short Bowel Syndrome
Even after my ileostomy was reversed, I had limited bowel control. I was in and out of the hospital for over a year, and in November 2013 I was diagnosed with short bowel syndrome or SBS. SBS is a rare, serious and chronic malabsorption disorder that occurs when parts of the intestine are removed, and the remaining intestine may not be able to absorb enough nutrients from food and drink. In adults, SBS can develop from a loss of function and surgical removal of parts of the intestine due to inflammatory bowel disease (IBD), such as Crohn’s disease. I sat there in shock. The thought of living like this for the rest of my life left me numb. When we returned home. I immediately went online. The more I read, the more I was worried. But then I realized, I could do this. Yes, having SBS would impact my life more than I initially thought, but it wouldn’t stop me.
At that time, since I could barely take care of myself, my husband had to stay at a nursing home.
My life was a roller coaster, out of control. I was confined to home by SBS. I would eat and have to use
the bathroom five minutes later.

I told my doctor, “I can’t live like this; this isn’t living. I don’t see my friends. I’m crying all the time.” Because I wasn’t able to absorb food or nutrients, I was placed on different forms of parenteral support, or PS. Monday through Saturday I had a large bag of clear saline solution and I had to administer the medications into the bag. The transfusion took 12 hours to complete. Then I had total parenteral nutrition (TPN) infusions at night. The infusions really limited my ability to get out of the house and be active. And when I did get out, I had to pack an emergency bag whenever I left the house in case I had an accident. I had cleaning supplies, garbage bags for soiled clothes, and clean clothing. It was so embarrassing having an accident when out with friends, shopping, going to the doctor, going to the dentist, going to the grocery store, mowing the lawn, or even talking to my neighbors. I didn’t know whether I should laugh or cry. I chose laughter because I was afraid to cry.
Starting An SBS Treatment
In May 2015, my determination and optimism were about at their limit when my doctor told me about a medication called GATTEX® (teduglutide) for subcutaneous injection. He told me I might be a good candidate to try GATTEX, which is a prescription medicine approved for use in adults and children 1 year of age and older with short bowel syndrome who need additional nutrition or fluids from intravenous (IV) feeding. This type of IV feeding is also known as parenteral support (PS). It is not known if GATTEX is safe and effective in children under 1 year of age.
We talked about the potential benefits and risks of the medication, including the risk of serious side effects including making abnormal cells grow faster, polyps in the intestines, blockage of the bowel (intestines), swelling (inflammation) or blockage of the gallbladder or pancreas, and fluid overload. Learning about these potential side effects led me to hesitate a bit, but I believed that if I didn’t try to treat my condition, it would remain the same or could even get worse. These are not all the possible side effects, so anyone considering GATTEX treatment should talk to their own healthcare professional or medical team. I weighed the risks and benefits, and my doctor and I decided together that I should start GATTEX.
Please continue reading for additional Important Safety Information.

Within six months, I was able to reduce my parenteral support (PS) with GATTEX, which meant less PS at night—with fewer accidents and more sleep. While this was my experience with GATTEX, others may have different treatment experiences. I still sometimes have uncontrolled bowel movements and I sleep on a pad. Because I still never know when an uncontrolled bowel movement may happen, I wear a pad if I’m going to be out of the house for a while, just in case. But I no longer have to carry a PS backpack with me. After being on GATTEX for a number of months, with the help and monitoring of my doctor, I was able to come off my PS. With less PS I was able to do things I enjoy.
I admit, I don’t love giving myself a shot every day. I always hesitate for a nanosecond and then surprise myself. Some days are easier than others. I do my shot at bedtime and rotate it around the four sections of my abdomen.
I can’t adequately describe my joy that GATTEX has worked well for me! Sure, I still have problems now and then, but really, who doesn’t have problems in life? It’s such a relief that I can leave home and enjoy the things I love! I travel, visit friends, go to the grocery store, play pickleball, and even golf!

If you’re diagnosed with SBS, don’t give up. There are times when I took life an hour at a time. I’d encourage you to focus on going forward. In my experience, it helps to have supportive friends and family, and a trusting relationship with the medical team helping you. My doctor has dietitians on staff and they work with my nutrition plan to help ensure I’m making good choices. My doctor orders tests to check my levels. If any of the results are “off,” I’m then advised of any changes that need to be made.
Today, I’ve hung up my Olympic medal for the bathroom dash and that’s just fine with me. I’ve faced the difficulties of living with short bowel syndrome and once again discovered hope, persistence, and laughter.
IMPORTANT SAFETY INFORMATION
What is the most important information I should know about GATTEX? GATTEX may cause serious side effects, including:
Making abnormal cells grow faster
GATTEX can make abnormal cells that are already in your body grow faster. There is an increased risk that abnormal cells could become cancer. If you get cancer of the bowel (intestines), liver, gallbladder or pancreas while using GATTEX, your healthcare provider should stop GATTEX. If you get other types of cancers, you and your healthcare provider should discuss the risks and benefits of using GATTEX.
Polyps in the intestines
Polyps are growths on the inside of the intestines. For adult patients, your healthcare provider will have your colon and upper intestines checked for polyps within 6 months before starting GATTEX, and have any polyps removed. To keep using GATTEX, your healthcare provider should have your colon and upper intestines checked for polyps at the end of 1 year of using GATTEX.
For pediatric patients, your healthcare provider will check for blood in the stool within 6 months before starting GATTEX. If there is blood in the stool, your healthcare provider will check your colon and upper intestines for polyps, and have any polyps removed. To keep using GATTEX, your healthcare provider will check for blood in the stool every year during treatment of GATTEX. If there is blood in the stool, your healthcare provider will check your colon and upper intestines for polyps. The colon will be checked for polyps at the end of 1 year of using GATTEX.
For adult and pediatric patients, if no polyp is found at the end of 1 year, your healthcare provider should check you for polyps as needed and at least every 5 years. If any new polyps are found, your healthcare provider will have them removed and may recommend additional monitoring. If cancer is found in a polyp, your healthcare provider should stop GATTEX.
Blockage of the bowel (intestines)
A bowel blockage keeps food, fluids, and gas from moving through the bowels in the normal way. Tell your healthcare provider right away if you have any of these symptoms of a bowel or stomal blockage:
- trouble having a bowel movement or passing gas
- stomach area (abdomen) pain or swelling
- nausea
- vomiting
- swelling and blockage of your stoma opening, if you have a stoma
If a blockage is found, your healthcare provider may temporarily stop GATTEX.
Swelling (inflammation) or blockage of your gallbladder or pancreas
Your healthcare provider will do tests to check your gallbladder and pancreas within 6 months before starting GATTEX and at least every 6 months while you are using GATTEX. Tell your healthcare provider right away if you get:
- stomach area (abdomen) pain and tenderness
- chills
- fever
- a change in your stools
- nausea
- vomiting
- dark urine
- yellowing of your skin or the whites of your eyes
Fluid overload
Your healthcare provider will check you for too much fluid in your body. Too much fluid in your body may lead to heart failure, especially if you have heart problems. Tell your healthcare provider if you get swelling in your feet and ankles, you gain weight very quickly (water weight), or you have trouble breathing.
The most common side effects of GATTEX include:
- stomach area (abdomen) pain or swelling
- nausea
- cold or flu symptoms
- skin reaction where the injection was given
- vomiting
- swelling of the hands or feet
- allergic reactions
The side effects of GATTEX in children and adolescents are similar to those seen in adults. Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
What should I tell my healthcare provider before using GATTEX?
Tell your healthcare provider about all your medical conditions, including if you or your child:
- have cancer or a history of cancer
- have or had polyps anywhere in your bowel (intestines) or rectum
- have heart problems
- have high blood pressure
- have problems with your gallbladder, pancreas, kidneys
- are pregnant or planning to become It is not known if GATTEX will harm your unborn baby. Tell your healthcare provider right away if you become pregnant while using GATTEX.
- are breastfeeding or plan to It is not known if GATTEX passes into your breast milk. You should not breastfeed during treatment with GATTEX. Talk to your healthcare provider about the best way to feed your baby while using GATTEX.
Tell your healthcare providers about all the medicines you take, including prescription or over-the counter medicines, vitamins, and herbal supplements. Using GATTEX with certain other medicines may affect each other causing side effects. Your other healthcare providers may need to change the dose of any oral medicines (medicines taken by mouth) you take while using GATTEX. Tell the healthcare provider who gives you GATTEX if you will be taking a new oral medicine.
Call your doctor for medical advice about side effects. You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
What is GATTEX®?
GATTEX® (teduglutide) for subcutaneous injection is a prescription medicine used in adults and children 1 year of age and older with Short Bowel Syndrome (SBS) who need additional nutrition or fluids from intravenous (IV) feeding (parenteral support). It is not known if GATTEX is safe and effective in children under 1 year of age.
For additional safety information, click here for full Prescribing Information and Medication Guide, and discuss any questions with your doctor.
Editor’s Note: This educational article is from one of our digital sponsors, Takeda. Sponsor support along with donations from our readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.
©2025 Takeda Pharmaceuticals U.S.A., Inc. 1-877-TAKEDA-7 (1-877-825-3327). All rights reserved.
Takeda and the Takeda logo are trademarks or registered trademarks of Takeda Pharmaceutical Company Limited.
GATTEX and the GATTEX logo are registered trademarks of Takeda Pharmaceuticals U.S.A., Inc. US-TED-1644v1.0 08/25










 kids saying “your mom would be able to kill all of those players” and when the kids saw that they were casting season 2, they begged me to apply. I just assumed my application would be lost in the thousands of emails, but fortunately something caught their attention!
kids saying “your mom would be able to kill all of those players” and when the kids saw that they were casting season 2, they begged me to apply. I just assumed my application would be lost in the thousands of emails, but fortunately something caught their attention!




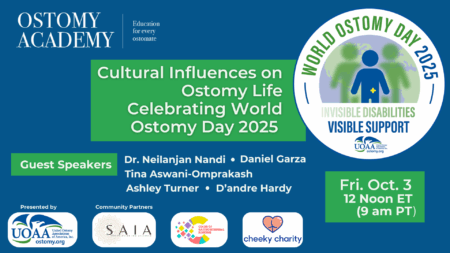 To kick-off the weekend events and celebrate World Ostomy Day UOAA is partnering with the nonprofit organizations
To kick-off the weekend events and celebrate World Ostomy Day UOAA is partnering with the nonprofit organizations 
 often overlooked, even within the wider disability movement. Having an ostomy has shaped so much of my lived experience, and I know how isolating it can feel when society erases or
often overlooked, even within the wider disability movement. Having an ostomy has shaped so much of my lived experience, and I know how isolating it can feel when society erases or 








