By Cheryl Ory, UOAA President
President Biden has proclaimed March 2023 National Colorectal Cancer Awareness Month. The American Cancer Society says that colorectal cancer is the third leading cause of cancer related deaths in both men and women. On another note, the death rate has been dropping for several decades. One reason is that treatments have improved. Another reason is that colorectal polyps are now being found more after screening and removed before they can turn into a cancer.

UOAA Advocate, ostomate and colorectal cancer survivor Allison Rosen speaks on the National Mall as part of the United in Blue Rally sponsored by Fight Colorectal Cancer. Video: United in Blue Rally on the Mall (1)
In 2008 I was diagnosed with Stage 3b colorectal cancer. I was told the cancer had been developing for at least 10 years or more, most likely when I was in my early 30’s. There was a polyp, if it had been removed at an earlier date the cancer would not have developed. After radiation, chemo, surgery, and more chemo I am now a colorectal cancer survivor with a permanent colostomy, an ostomy that has saved mine and others lives from not only cancer, but other debilitating diseases.
I’m happy that UOAA is standing alongside partner organizations like Fight Colorectal Cancer to push lawmakers into giving attention to the alarming rise in young people with colorectal cancer.
With younger people being as risk and diagnosed , The U.S Preventative Services Task Force lowered the recommended screening age to 45 in 2021. One in five colorectal cancer patients is between the ages of 20-54. Talk to your doctor about options for colorectal cancer screening. As the Colon Cancer Coalition states with earlier screening and detection, “Colorectal Cancer can be Preventable, Treatable, Beatable.”
If you are a person still at risk, like those with IBD, let me urge you to get screened. Screening can result in any colorectal cancers being found earlier when they are easier to treat.
Here at United Ostomy Associations of America (UOAA) we have a long legacy of supporting the survivors of cancer and many other conditions so that they can have best quality of life possible. If your cancer requires a life-saving ostomy surgery remember-you are not alone. 725,000- 1 million people in the U.S. of all ages and backgrounds live with an ostomy.
 Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary ileostomy (from the small intestine) or colostomy (large intestine). This may be required to give a portion of the bowel a chance to rest and heal. When healing has occurred, the colostomy can often be reversed and normal bowel function restored. It’s important to know that not everyone with an ostomy will be a candidate for a reversal operation. A permanent colostomy may be required when a disease affects the end part of the colon or rectum.
Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary ileostomy (from the small intestine) or colostomy (large intestine). This may be required to give a portion of the bowel a chance to rest and heal. When healing has occurred, the colostomy can often be reversed and normal bowel function restored. It’s important to know that not everyone with an ostomy will be a candidate for a reversal operation. A permanent colostomy may be required when a disease affects the end part of the colon or rectum.
We have new Living with a Colostomy guide and ileostomy guide to help you learn as much as possible before or after you have this life changing surgery.
It’s especially important to connect with one of hundreds of UOAA Affiliated Ostomy Support Groups in the U.S. before, or shortly after, your surgery. Peer support and preparation can put you on the path to success in what may be a challenging time both emotionally and physically. Ask if the hospital has a certified ostomy nurse and insist on having your stoma placement marked before surgery. These and other self-advocacy tools are paramount and outlined in our Ostomy Patient Bill of Rights.
You may feel too overwhelmed as you are discharged at the hospital to fully understand ostomy pouching systems and accessories and lifestyle considerations. If you have a medical question contact your doctor or nurse, but if you have a quality of life question-UOAA resources here at ostomy.org and peers at UOAA Affiliated Support Groups likely have the answers.
It’s important to learn the facts about living with an ostomy. After the healing period outlined by your surgeon you can swim, bathe, be intimate, travel, and embrace a new normal life. After some trial and error, you may also eat most of the foods you have been able to eat in the past. Education is key to battling misinformation.
Unfortunately misinformation and stigmas surrounding both ostomy surgery and colorectal cancer affect the number of people getting screened or getting the medical treatment they need. Let’s work together to educate, advocate and support survivors.
Cheryl Ory is a colorectal cancer survivor who received a permanent colostomy in 2008. Cheryl is a Registered Nurse who has had a passion for volunteering with the ostomy community ever since and first joined UOAA’s Board of Directors in 2015. She now holds the position of President.
For people who have recently come to accept or are still struggling to manage one ostomy the news that they may need to have a second stoma and pouching system could be overwhelming. Please know you are not alone. Many people are able to thrive in life with two ostomies, or multiple diversions.
When UOAA hears from those with questions for a double ostomate we often refer them to ostomy community friend Jearlean Taylor. Jearlean wanted to share some advice and invite all double ostomates to her talk and open discussion entitled “Life as a Double Ostomate” on August 12, 2023 as part of UOAA’s National Conference in Houston, Texas.
Sharing with the community of double ostomates is so refreshing and exciting. It is true “we are not alone”. We can live our life as a double ostomate with joy.
I am Jearlean from Baltimore, Maryland. I am a double ostomate, fashion model, author, motivational speaker, entrepreneur, and ostomy advocate.

My life has had some unexpected outcomes. I guess you can say “life” happened. At the tender age of 3 years old I developed a rare form of cancer (Rhabdomyosarcoma). Because of the tumors I had to undergo ostomy surgery, which left me with two permanent ostomies (colostomy & urostomy).
If you or a child come to find you need a second ostomy my advice is to ADAPT. I had to learn to adapt. As I got older it was two major things for me to adapt; body and mind. When we hear two ostomies we get scared, but when we accept what we can’t change it says we are survivors. I adapted to new ways of taking care of my body (ostomies) and keeping my mind positive. Those still adapting to having two ostomies reflect how far you have come and where you are now. Celebrate each moment.
A Common question or statement I get is “you had your ostomies that long. How did you adapt?” The moment I learned to deal with my medical circumstance when my mom explained that I was not different from anyone else. I am beautiful with my bags. I can be, do, and follow my passions and dreams. I can live a full and vibrant life. It happened just as she said. Because of what she instilled in me, I BELIEVED IT.
When we hear two ostomies we get scared, but when we accept what we can’t change it says we are survivors.
Sharing with the community of double ostomates is so refreshing and exciting. It is true “we are not alone”. We can live our life as a double ostomate with joy. We are more than our ostomies.
I also try to give encouraging tips for dressing with an ostomy for comfort and peace of mind. Remember.
- We are beautiful from the inside out
- Work with your body type and comfort
- Look for clothing that YOU like ,and what is comfortable for your ostomies
- Shopping for clothing; take a family or friend along for support
- Try on multiple items of clothing, even the clothing in your closet
- Consider ostomy accessories (ostomy wraps, stealth belt, hernia belt, fitted tops, high waist undergarments, etc..)

We have the ability to make a difference and change lives even through our struggles. You may have an ostomy, dealing with chronic illness, feeling down and inadequate at times, but remember you are more than you have become. Our situations, challenges, and unforeseen circumstances does not have to dictate who we are or who we can become. My purpose is to inform everyone that “life” happens to us all; good, bad, and indifferent. I want to show people even through our struggles, pain, disease, and even having ostomy we have a purpose in life.
“DIFFERENT TO MAKE A DIFFERENCE“
You can find Jearlean online at jearleantaylor.com and across social media. Meet her and a whole community of double ostomates at UOAA’s 8th National Conference August 10-12, 2023, In Houston Texas.
By UOAA Advocacy Manager Jeanine Gleba, MEd.
For several years UOAA has been advocating for those in the ostomy and digestive disease communities who use opioids for non-pain conditions. In UOAA’s May 2022 ENewsletter we reported that UOAA submitted federal comments with the National Center for Injury and Prevention and Control at the Centers for Disease Control and Prevention on its draft update of the 2016 CDC Guidelines for Prescribing Opioids for Chronic Pain. We recommended that the guidelines should not be intended for primary care physicians and other clinicians providing non-pain care for outpatients such as those with digestive diseases resulting in an ostomy or fecal continent diversion who may use opioids to manage high output stomas or patients with short bowel syndrome.
On November 4th, the CDC released the updated Clinical Practice Guidelines for Prescribing Opioids for Pain – United States, 2022. They had over 5500 public comments submitted.
Our voices were heard! In the CDC Response to Public Comments on the Draft 2022 Clinical Practice Guideline for Prescribing Opioids for Pain they specifically mention our submission under the “summary of themes that emerged from the public comments submitted to CDC” bullet number six:
- Some respondents representing non-pain related conditions that use opioids for treatment (e.g., ostomy-related conditions and restless leg syndrome [RLS]) proposed that the Guideline title should be adjusted to better reflect its content and intended use.
Then on page 4 under the “summary of edits the CDC made to the draft 2022 Clinical Practice Guideline based on public comment” bullets 2 and 3 apply to our comments and concerns:
- CDC changed the name of the document from the CDC Clinical Practice Guideline for Prescribing Opioids to CDC Clinical Practice Guideline for Prescribing Opioids for Pain to further emphasize its focus on prescription opioids for the treatment of pain.
- CDC added language throughout the document to emphasize that the 2022 Clinical Practice Guideline provides voluntary clinical practice recommendations that are not intended to be inflexible standards of care or implemented as absolute limits of policy or practice for patients by clinicians, healthcare systems, or government entities.
They did not specifically add any statement that the guidelines are not intended for primary care physicians and other clinicians providing non-pain care for outpatients with chronic and acute digestive diseases; however, the important takeaways from the document for our patient population are the following:
1) The voluntary guideline is intended ONLY for primary care clinicians and other clinicians providing PAIN care (acute pain, subacute pain and chronic pain).
2) The guideline is not a replacement for clinical judgment or individualized person-centered care.
3) The guideline should not be applied as inflexible standards of care across patients or patient populations by healthcare professionals, health systems, pharmacies, third-party payors or state, local or federal organizations or entities.
4) The guideline is not a law, regulation or policy that dictates clinical practice.
5) As stated on page 5 – “To avoid unintended consequences for patients, this clinical practice guideline should NOT be misapplied, or policies derived from it, beyond its intended use. Examples of misapplication or inappropriate policies include being inflexible on opioid dosage and duration, discontinuing or dismissing patients from a practice…and applying recommendations to populations that are not a focus of the clinical practice guideline.”
In conclusion, it is clear that these new guidelines should not be applied to our patient populations utilizing opioids for non-pain treatments in accordance with the recommendations of their physician, which was the goal of our advocacy effort.
With the updated CDC guidelines there should no longer be any misinterpretation of their voluntary recommendations. Our patient community will be protected and should not be restricted access to their lifesaving treatment.
.
By Ed Pfueller, UOAA Communications Manager
Taylor Mitchell and Michael Ross
It was raining every day, for weeks, before Taylor and Michael were set to get married. But as the recently wed couple stepped out of the church for photos, only the sun was shining, a distant mountain range framed their joy – the chilly Alaskan rain held off.
shining, a distant mountain range framed their joy – the chilly Alaskan rain held off.
“It was an absolutely magical day,” says Taylor, the bride. “Taylor took my breath away when I saw her, she was absolutely stunning,” Michael recalls.
Even if the dark clouds had drenched their special day, it’s doubtful it would have dampened their mood. This specific couple is used to living with ostomies and chronic illness and they seem prepared to weather any storm.
Friends from the Start
Taylor and Michael first met ten years ago in a local college undergrad class. “I scanned the room, saw him, thought he was cute, and decided I wanted to sit by him and try to be friends. I didn’t know if anything would come of our friendship. We had a great connection as friends, Taylor recalls.
“She was smart, insightful, and easy on the eyes, but I would never have imagined she was interested in me beyond friendship,” Michael says.
The friendship slowly turned into dating. “We have a lot in common and also have a lot of differences. I love to plan, and she is more spontaneous. We both respect each other and can be vulnerable with each other, and the biggest thing is we trust each other,” Michael says.
Taylor says some things she loves about Michael is that he understands her and that they have a shared faith. “He always wants to help me any way he can, and he’s generous to others,” she says.
What is an Ostomy?
“While we were dating, I didn’t know Michael had an ostomy for a while and when he did tell me, I had no idea what it was,” Taylor says. “His ostomy was never an issue for me and so my experience while dating was positive! His ostomy never impacted anything in our relationship from my perspective.”

Michael has had a long ostomy journey and awareness, his mother had a urostomy. ”I had a colostomy for about two years, takedown for four, and have had a permanent ileostomy for the past fifteen years due to complications with Crohn’s disease,” he says.
“I didn’t date much before I met Taylor but had no negative experiences when I did date. Taylor was very understanding when I told her (and showed her) about my ostomy. She was very understanding and seemed eager to learn more.”
“My advice would be, if you’re a person who doesn’t have an ostomy and finds yourself dating someone with an ostomy, educate yourself and do your best to understand your partner, their limitations (if any), and then just treat them as a regular person!” Taylor says.
Taylor also advises that if you have an ostomy and find yourself with someone who doesn’t have an ostomy. “Give the partner an opportunity to accept you and make the choice for themselves on what they’re comfortable with. You’re not for everyone and that’s ok and vice versa! I think it will always be slightly nerve-wracking to have a body that isn’t “normal” by current beauty standards because of the fear of rejection and embarrassment, Taylor says. “Society tends to tell us that no one will want us if there’s something “wrong” with us. But, if you can muster the courage to put yourself out there, the outcome may be better than you ever imagined!”
I don’t think we will have any more challenges than the average couple… we just poop differently. -Michael Ross
In Sickness and in Health
 Caregiving has been a consistent part of Taylor and Michael’s relationship. “When Michael had to have revision surgery, I wanted to make sure he’d have easily accessible food so he could focus on healing. I came over to his house prior to surgery and we made a few different meals to freeze. It was a great feeling for me that we got to spend time together cooking and his food would be taken care of while he recovered. He was used to taking care of himself so it meant a lot to me to do this for him.”
Caregiving has been a consistent part of Taylor and Michael’s relationship. “When Michael had to have revision surgery, I wanted to make sure he’d have easily accessible food so he could focus on healing. I came over to his house prior to surgery and we made a few different meals to freeze. It was a great feeling for me that we got to spend time together cooking and his food would be taken care of while he recovered. He was used to taking care of himself so it meant a lot to me to do this for him.”
Meanwhile, Taylor started dealing with her own undiagnosed chronic illness. “I had to go to the Mayo Clinic while we were dating, and he took time off of work to come with me for a week. He came to all my appointments and helped me navigate all my emotions with what I was dealing with. This is the kind of thing we do for each other, we try to make the hard times easier by taking care of the small things and the big things,” she says.
Just a year and a half ago Taylor, with her health worsening Taylor had ostomy surgery as a result of chronic constipation. For better or worse they were now an ostomate couple.
A Couple of Ostomates
After her ostomy surgery, Taylor says she, “shared with him every single aspect of what I was going through. It was nice to be with someone who already knew! It felt good from my perspective to understand him better, now that we had the same appliance… I actually knew first-hand what he was dealing with.”
Michael says that one of the best parts of being with another ostomate is knowing that someone really understands what you are going through. “It’s nice to be able to compare notes on new products and understand when my partner isn’t feeling well, to have the option to share supplies, tag along to doctor’s appointments, and ask questions about care, procedures, and recovery,” he says.
In addition to a new mutual understanding of health issues, Taylor says, “We know what to do if one of us isn’t feeling well. We just understand each other on a deeper level. He accepts me as an individual and he accepts my body even as it changes with all my health challenges.”
It felt good from my perspective to understand him better, now that we had the same appliance… I actually knew first-hand what he was dealing with. -Taylor Mitchell
As for difficulties, they both dread a possible double leak at night, and can imagine the challenge of not feeling well at the same time or needing a procedure around the same time. Taylor says the most challenging part has been encouraging the other to stick to the foods that work for us, to drink water more consistently, and get our electrolytes in.” Michael concludes, “I don’t think we will have any more challenges than the average couple… we just poop differently.”
Finding Community and Support
 Even with partner support, Taylor says “UOAA has been so incredibly important to me in my ostomy journey. When I first got my ostomy, I scoured the UOAA website and read every piece of information I could find which helped ease my mind and answer my questions. UOAA’s website also helped me to be able to share information about my ostomy with family and friends.”
Even with partner support, Taylor says “UOAA has been so incredibly important to me in my ostomy journey. When I first got my ostomy, I scoured the UOAA website and read every piece of information I could find which helped ease my mind and answer my questions. UOAA’s website also helped me to be able to share information about my ostomy with family and friends.”
The couple, who both work in logistics, has recently moved to Colorado but while in Alaska both say they had the good fortune of having Luella Odmark as their WOC nurse.
“Luella is an amazing individual who cares so deeply about ostomates,” Taylor says. She does a training for nurses at one of our hospitals and has invited my husband and I to speak to the class about our ostomy history, give advice on what we wish we had from nurses, doctors, and hospital staff as well as sharing some of our favorite products,” she adds.
“I enjoyed observing the transformation of two people pursuing their own interests, coming together, including getting married, now mentoring others about ostomies,” says Odmark, a WOC Nurse and the leader of the Anchorage Ostomy Support Group. “I hope to see them continue to spread hope about living with an ostomy,” Odmark adds.
Odmark also joins the couple each Ostomy Awareness Day to walk the Run for Resilience Ostomy 5k. The experience was especially meaningful to Taylor. “The Ostomy 5k was a huge accomplishment the first time I did it because I was three months post op and it was a huge struggle for me to walk a 5k, I almost didn’t finish it and wanted to give up so many times. Taylor continues, “My second time, this year, it was still a hard thing for me to accomplish but I did so much better! I loved seeing people from all over doing their 5k however was comfortable for them. It was encouraging!”
UOAA has been so incredibly important to me in my ostomy journey. -Taylor Mitchell
Taylor is especially open about her ostomy journey and embraces Ostomy Awareness Day as a chance to connect with more people online and see their stories. “It’s such a nice feeling to know that I am not alone. I see people who are confident with their ostomy and I see people who are working to build their confidence,” Taylor says.
Taylor hopes to help even more people and nurses through UOAA outreach opportunities. “I love UOAA’s mission, I love the work they do, and I love all the resources that are available for FREE so financial barriers are removed for as many people as possible. Accessibility is so important! I am proud to be a supporter of UOAA.”
Michael agrees and adds, “I’m very thankful for all of the people that organize the walk, work with ostomates, and are around to help us on our ostomy journey. I’m most thankful for my wife, who I get to take this journey with every day.”
Excerpts from Matthew Perry’s new memoir show that even TV stars are vulnerable to poor ostomy care and stigmas UOAA is working to erase.
By James Murray, UOAA President
(Update: People around the world have been reacting to the sad news that Perry was found dead in his home on October 28, 2023.)
In a preview of his new memoir Friends star Matthew Perry reveals to People that in 2019 his colon burst from opioid abuse and that he spent two weeks in a coma before waking up unaware that he had emergency ostomy surgery to save his life.
He reveals that ‘It was pretty hellish having one because they break all the time’ which as President of United Ostomy Associations of America (UOAA) shows me that even a Hollywood star is susceptible to poor quality of care and the ostomy stigmas our organization is fighting to end.
I had lifesaving ostomy surgery as a result of colon cancer and I am among the 725,000 to 1 million people in the United States we estimate are living with an ostomy or continent diversion. Many of us live healthy and active lives thanks to follow-up care by certified ostomy nurses, education, emotional support, and the fact that a properly fitted ostomy pouch should not break, smell or restrict your desired lifestyle.
The book also reveals that Perry’s ostomy was temporary and that his therapist said ‘The next time you think about taking OxyContin, just think about having a colostomy bag for the rest of your life.’ Perry says this was the catalyst for wanting to break his long pattern of addiction.
While it’s wonderful that Perry has fought to end his addiction, these words sting for those of us who deal with the consequences of ostomy stigmas in our society. We wonder if Perry would have come to see the ostomy differently if given the chance to attend an ostomy support group or talk with another person living with an ostomy during his 9-month recovery. Did he receive information about organizations that support ostomy patients prior to discharge? Research shows that these and other UOAA standards of care can make all the difference in a patient’s outcome.
Despite the fact that ostomy surgery saves or improves lives, there are still people who believe that death is a better choice than having this surgical procedure. People of all ages struggle with body image issues and acceptance in life with an ostomy and perpetrating these stigmas can leave deep scars.
Perry also mentions looking at the scars from his 14 abdominal surgeries as motivation for ending a cycle of addiction. Perry and those interviewing him are rightly celebrating and supporting addiction recovery efforts. We ask that they also give a moment to help raise positive ostomy awareness, and share our resources available to all those in need.
James Murray is President of United Ostomy Associations of America Inc. (UOAA) a national 501(c)(3) nonprofit organization that promotes quality of life for people with ostomies and continent diversions through information, support, advocacy and collaboration. Educational resources, advocacy tools, support groups and more can be found at www.ostomy.org)
Donate today to help the next ostomate in need.
UOAA Research Results Are Published Showing Patient Rights Are Being Utilized but Gaps in Care Being Provided Exist
By Jeanine Gleba, UOAA Advocacy Manager
Everyone in the United States has the right to receive high quality care. However, the ostomy community continues to be plagued by poor quality care due to lack of trained medical professionals such as certified ostomy care nurses. Many caring for a person with an ostomy do not have the education related to the physical, emotional or quality of life needs of someone living with an ostomy. Thus, those in the ostomy community often feel a lack of compassion and respect regarding their care. UOAA receives hundreds of calls and email inquiries annually, many of them desperately seeking assistance for proper ostomy care.
It is a primary mission of UOAA advocates to assure that quality ostomy care occurs universally across all health care settings.
In 2019 UOAA embarked on a research journey to examine best-in-practice care for ostomy patients through the utilization of the Ostomy and Continent Diversion Patient Bill of Rights (PBOR), which are evidence-based for quality ostomy care. We wanted to know if these written standards are the accepted practiced norms for treatment and care for ostomates.
Together let’s establish a culture that promotes the highest quality care for ostomates.
We collected data from both ostomy surgery patients (412 respondents) and medical clinicians (195 respondents) such as Wound Ostomy Continence nurses. The organization is thrilled to announce the release of our research results that were published in the September/October 2022 issue of the Journal of Wound Ostomy Continence Nursing.
There were three research questions that the study investigated
- Is UOAA’s PBOR being used to care for ostomy patients analyzed from the perspective of patients and clinicians?
- Do patients and clinicians perceive that use of the PBOR is beneficial to ostomy patient health outcomes?
- Have clinicians witnessed positive patient health outcomes (e.g., decreased readmissions for dehydration, feeling better prepared to care for the ostomy)?
Promising findings showed that, for the clinicians familiar with the PBOR, more than half reported that the PBOR was being utilized to inform ostomy care1. Additionally, a majority of both patients and clinicians indicated that consistent use of the PBOR may be beneficial for ostomy patient health outcomes such as prevention of Emergency Department visits1. However, analysis identified a significant gap in specific standards of care being provided by clinicians versus the care patients reported they received1. For example, 22.5% of the patient population reported engaging in a discussion on the emotional impact of the ostomy surgery versus 65.6% of the clinician respondents reported it was provided1. Another notable difference was the number of patients (55.1%) who reported receiving educational materials specific to ostomy care versus 82.5% of clinicians reported providing educational materials.

The study concluded that there are discrepancies between PBOR standards of care being provided by clinicians versus the care patients reported they received. Further awareness and wider utilization of the PBOR are needed to provide best care to patients living with an ostomy1.
Advocacy work is ongoing and quality health care is a team effort. Together let’s establish a culture that promotes the highest quality care for ostomates. When quality of care is not provided, people should speak up. The more people that demand these rights and the more medical professionals who perform these standards of care, the more improvements will be realized in patient care and outcomes.
1.Gleba, Jeanine; Miller, Leslie Riggle; Peck, B. Mitchell; Burgess-Stocks, Joanna. United Ostomy Associations of America's Ostomy and Continent Diversion Patient Bill of Rights: An Examination of Best-in-Practice Care for Ostomy Patients. Journal of Wound, Ostomy and Continence Nursing: September/October 2022 - Volume 49 - Issue 5 - p 462-468 doi: 10.1097/WON.0000000000000909
By Ed Pfueller, UOAA Communications and Outreach Manager
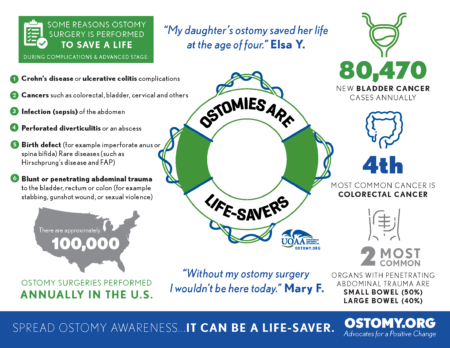
The ostomy community is a big group with diverse medical backgrounds, ages, and attitudes about living with an ostomy. One thing almost everyone can agree on is that ostomy and continent diversion surgery saves lives. We all hope for a day when no one who has an ostomy feels alone in life. Ostomy Awareness Day is Saturday, October 1, 2022 and however you are most comfortable participating – you can have an impact. Your voice matters and now is the time to use it or support others who do.
If You’re Supportive but Busy

I had very little to go on, more to learn than I realized, and felt somewhat lost and well, scared. Discovering United Ostomy Associations of America (UOAA) when searching online for ostomy organizations and associations was a relief and godsend. -Myrna Pair
A couple of clicks is all it takes to put a smile on the face of a resilient ostomate or dedicated ostomy nurse. Check out the heartwarming stories of those on the Run for Resilience fundraising pages. Many of them still need a donation. The Ostomy 5k is the biggest fundraiser of the year for the programs and services offered by UOAA, a national 501 (c)(3) nonprofit organization. We have not met the Virtual Ostomy 5k fundraising goal of $25,000. Donating to UOAA, whenever you have the means, helps to sustain our small but powerful national ostomy organization’s work to improve the quality of life for people living with an ostomy, all year long.
If You’re Active on Social Media
Great, stop scrolling and go share your #OstomiesAreLifesavers story today! Even if you have never talked about it publicly before, consider letting your social networks know the things you have been able to do and witness in life after surgery. Help dispel stigmas and fear surrounding ostomy surgery, you never know which of your connections may have an ostomy or be faced with surgery someday. Post a photo, video or story and tag or DM @UOAA and use the hashtag #OstomiesAreLifesavers and #OstomyDay2022
Another quick and easy way to share your ostomy story is to complete the This or That Ostomy Edition, tag uoaa and post it to your stories.
If You’d Rather Work Behind the Scenes
You don’t have to post ostomy bikini pics to be an effective advocate. Anyone can call or send our action alerts to their elected officials. The U.S. Congress has designated official days for mountain biking and cowboys but not for Ostomy Awareness. This is because of a lack of congressional co-sponsors. Congressman Donald Payne (NJ) is introducing a Congressional House Resolution designating October 1, 2022 as National Ostomy Awareness Day and needs co-sponsors and/or support for this resolution. Contact your Congressperson and ask them to become a cosponsor, by contacting Shahryar M. Baig on his staff at shahryar.baig@mail.house.gov. You can take action here on all of our advocacy campaigns.

These @delta #flightattendants and #pilot were 100% on board to support #OstomyDay2022 – Peenelopie was very excited that the pilot got to hold her! (courtesy Stomagienics)
If You Just Want to Have Some Fun While Raising Awareness
Consider printing out our Ostomy Pouch Character name it, and take pics of it wherever you go Flat Stanley style; send us your pics or post on social media. To make it even easier use our Giphy stickers found here (or search @UOAA_Ostomy)
You can still register for an in-person Run for Resilience Event near you on Saturday (Birmingham is Oct. 8) and join what is often a party atmosphere of music, sponsor tables, food and games – in addition to walking/running.
Also be sure to wear a stoma sticker from Hollister, the Exclusive Diamond Sponsor of UOAA’s Run for Resilience. Check out all the ways you can celebrate with Hollister.
If You Want to Get More Educated or Educate Others
If you want to get some WOC Nurse level information you’re in luck on October 1st. The WOCN Society is offering an education day event open to everyone free of charge.
For a more Ostomy 101 level of learning use our advocacy tools and infographics as a handout or post online. Feel free to use any of our materials on emotional support, ostomy myths, j-pouches or more.
The day after Ostomy Awareness Day you can also learn more about ostomies and mental health during a Facebook live event hosted by Crohn’s and Colitis Foundation in partnership with UOAA.
If You Want to Keep the Awareness Going All Month/Year Long
Here at UOAA we work on National Advocacy all year long. Sign-up for our advocacy action alerts and Monthly E-Newsletter. There is power in numbers, become a national individual member and be counted as an official member of UOAA’s ostomy community. You’ll also get a membership and stoma pin and among other benefits.
New this year, Convatec is planning “Ostober” to focus on ostomy awareness all month long. They are the Platinum Sponsor of our Run for Resilience Ostomy 5k and we’re thrilled to see them keeping the spirit alive all month long.
Visit our Ostomy Awareness Day landing page for more information this special day. Whatever you choose to do please let us know! If you have pictures, proclamations or stories to share send them to us at info@ostomy.org and don’t forget #OstomiesAreLifesavers
Written by Danielle Gulden and Joe Teeters
We all know that “laughter is the best medicine”! This year’s Ostomy Awareness Day Champions, Danielle Gulden and Joe Teeters, not only love that phrase, they live it! These two best friends, and co-founders of Double Baggin’ It are IBD warriors and permanent ileostomates. They’re also comedians, speakers and Two Best Friends without Buttholes! They truly believe in the power of laughter, humor, advocacy and awareness! Which is why they LOVE Ostomy Awareness Day! For them, every day is a chance to raise awareness. But Ostomy Awareness Day is a special day to reflect and celebrate their life-saving surgeries and the lives they were given back! They share their stories so that future, new and veteran ostomates know that they are not alone!
Danielle and Joe have each been living with Inflammatory Bowel Disease for over 29 years. Although their IBD and ostomy journeys have been quite different, their positive outlook on life and ridiculous sense of humor are the same!
Prior to 2014, Joe and Danielle had no idea the other existed…so, let’s rewind a few decades and learn about the journey of each of these Two Best Friends Without Buttholes!
Growing up, Danielle was a very healthy child, an extremely outgoing teen, and an adventurous free spirit! Spontaneity was her specialty, and travel was always her first love! Joe, on the other hand, always had “poop problems.” He was always pooping and known as “Joe the Pooper” by his siblings. Like Danielle, he was an outgoing, active, and social teenager.
Fast forward to Danielle’s late teens and early 20s. By the time she was a sophomore at The Ohio State University, Danielle’s health drastically changed! She saw her busy social life dissolve; she’d make plans and have to cancel. Spontaneity was no longer an option, and the idea of traveling was now a nightmare!
Danielle had to drop out of classes because of her poor health. Her symptoms and pain were becoming harder to ignore. She was in the bathroom around 25 times a day and became extremely malnourished and anemic.
You can hide your bag, but don’t ever let your bag hide you!
After being misdiagnosed for 6 years with a gluten intolerance, a colonoscopy in April of 1999 showed severe ulcerative colitis. From 1999 until 2007, Danielle’s life was a constant barrage of colonoscopies, radiological tests, bloodwork and pharmaceutical cocktails. She did the research and finally decided to have ostomy surgery.
After high school, Joe enlisted in the Naval Reserves. He passed the military physical and was cleared for training. While away, Joe’s poop problems became more pronounced, and the pain was gradually becoming more than just an annoyance.
When he returned home after 5 months, he was in the best physical shape of his life. On the outside he looked healthy, but inside something was wrong. Joe was initially diagnosed with irritable bowel syndrome, then a colonoscopy in 1993 lead to his diagnosis of severe Crohn’s Disease. Two years later he had his first intestinal resection. Joe’s Crohn’s continued to advance, and he had a second intestinal resection in October of 2004. 
Back in Cleveland, Danielle was super excited for her ostomy surgery! She was ready to stop being a prisoner to her bathroom and get back to living her life to the fullest! On April 30th, 2007, Danielle had her total proctocolectomy with end ileostomy at the Cleveland Clinic. It was truly one of the greatest days of her life! She high fived every single person on the way to the OR.
From day one, she embraced her ostomy, and her new life as an ostomate. Within a month or two of her surgery, Danielle was back to exploring and enjoying her pre-sickness hobbies and joys. She traveled, hiked, camped, swam, went to concerts, and amusement parks. Life was good again! She also joined the Cleveland chapter of the UOAA and eventually became active on their executive board.
Fast forward a few years, and 120 miles away in Columbus, Ohio. Within a year of his second resection, Joe’s rectal Crohn’s disease became severe, and his rectum very strictured. After consulting with his GI and surgeon, Joe had a full proctocolectomy with end ileostomy on December 27th, 2012.
Joe’s recovery process and post-surgical experience was very different from Danielle’s. In addition to becoming an ostomate, the amount of bowel he had lost from three surgeries left him with Short Bowel Syndrome. It took the better part of a year to fully recover and return to pre-surgery activities.
During Joe’s recovery, a Facebook support group for ostomates became a lifeline. It was a great source of inspiration and hope, and a wonderful place that showed him he was not alone. Later, he sought out Central Ohio United Ostomy Association support group and became a member of the organization.
By now, you must be wondering how the heck these Two Best Friends Without Buttholes finally met. As you can see, they have traveled separate but similar paths in their battles with Crohn’s and ulcerative colitis. Their paths crossed in that Facebook support group mentioned earlier, when Danielle posted that she and her family were relocating to Columbus, Ohio. Joe, being a Columbus resident, and fellow ostomate, reached out and introduced himself. After meeting in person, in late 2014, at their local UOAA Affiliated Support Group, they started hanging out after the meetings. They soon discovered that they had a very similar outlook on life and shared a ridiculous sense of humor, and they wanted to use that to help others. A best friendship began…and slowly but surely, their vision for Double Baggin’ It was coming together. They decided to go to the United Ostomy Associations of America’s National Conference in September of 2015. There, after meeting over 400 ostomy patients like themselves, they decided to stop dreaming and start making their vision for Double Baggin’ It a reality. Double Baggin’ It was born, that week, when they filmed their first DBI video on a rooftop in downtown St Louis, Missouri.
Through Double Baggin’ It, Danielle and Joe use their humor, wisdom, and stories to connect with and support other people living with ostomies and Inflammatory Bowel Disease. They advocate and raise awareness at the local and national level for both United Ostomy Associations of America and the Crohn’s and Colitis Foundation. Danielle and Joe also visit with their legislators yearly in Washington, DC to share their voices and stories.
You can find them on Facebook, Instagram, TikTok, Twitter and YouTube (@DoubleBagginIt) where you can watch them raise awareness through shenanigans and ostomy-bombing (placing an ostomy bag on a statue, landmark, anywhere they see fit!) They also can be found speaking at IBD and ostomy conferences, support groups, camps, hospitals and classrooms – sharing their stories and spreading laughter through improv. Danielle and Joe know that not everyone is comfortable rocking out with their bags out – and that’s totally ok! What these Two Best Friends Without Buttholes want to make perfectly clear, is that “You can hide your bag, but don’t ever let your bag hide you!”
Join with this year’s Ostomy Awareness Day Champions in spreading awareness by following Double Baggin’ It and UOAA on social media and visiting the Ostomy Awareness Day page to keep up to date on all the latest events.
Words and Photos by Jessica Miles
Living with a permanent ostomy can bring on significant changes in one’s personal, social and professional life. My biggest fear around having my ostomy surgery was leakage, particularly in public, skin breakdown and altered body image. There was a lot of trial and error in the beginning, but I have found what works for me as well as the confidence to share about it. I have always been an empath and very compassionate, however, I have now found a new passion for helping others (through my surgeon and on social media) learn how to manage their ostomy as well as how to cope with their new life. If you are willing and able to adapt, you can do anything!

In 2016, after years of unexplained symptoms, countless procedures, hospitalizations, tests, and a couple of misdiagnoses, it was confirmed that I had a genetic connective tissue disorder caused by a defect in the protein collagen. I was diagnosed with Classical type Ehlers-Danlos Syndrome. More than 90% of people with Classical EDS have mutations in the COL5A1 or COL5A2 gene. I have a mutation of the COL5A2 gene. The condition is inherited in an autosomal dominant manner. Treatment and management is focused on preventing serious complications and relieving symptoms.
Classical EDS is associated with skin hyperextensibility, joint laxity, fragile blood vessels, joint hypermobility, migraines, joint and muscle pain. Some individuals with this subtype have a deformity of heart valves and may experience a dilatation of the aorta. In cEDS there is also an increased risk for aortic dissection. cEDS patients are prone to hernias and organ prolapse, as well as comorbidities such as autonomic dysfunction…which regulates heart rate, blood pressure, temperature, pupillary response and digestion.
I ended up having multiple surgeries over the past four and a half years due to intestinal dysmotility, prolapses and hernias, resulting in a port and a permanent ostomy. I now, have an ascending end colostomy. While I prepared for years for the possibility of having one, I realized nothing truly prepares you for the actuality of living with a bag on your belly for the rest of your life. Though little by little, the stigma took a back seat to the reality that life with an ostomy can be just as good, if not better for some, than life without one. I suffered constantly from abdominal pain, nausea, vomiting, bloating, constipation, bowel obstructions and malabsorption. While I still struggle with many debilitating symptoms of my disorder, I am now able to eat, gain weight and go to the bathroom regularly. Something I always took for granted until I was no longer able to do so.
My symptoms aren’t usually visible to the untrained eye, but they are life-altering for me.
Though I have a constant physical reminder of my condition in the ostomy, to the rest of the world, mine is a largely invisible illness.
 It’s hard to describe how I feel to someone who has no idea what daily life with a chronic illness is like. I feel awful on the inside but look perfectly fine on the outside. Putting on a brave face for all to see has become a habit. My symptoms aren’t usually visible to the untrained eye, but they are life-altering for me.
It’s hard to describe how I feel to someone who has no idea what daily life with a chronic illness is like. I feel awful on the inside but look perfectly fine on the outside. Putting on a brave face for all to see has become a habit. My symptoms aren’t usually visible to the untrained eye, but they are life-altering for me.
I’ve learned to take everything step by step and day by day. My goal is to break down the stigma of ostomies, and while it’s not always easy, to show that one can still thrive and live a happy life with chronic illness. Due to pain and fatigue, I’ve learned to budget my energy, and while I may function normally one day, I usually need to rest the next. It’s all about finding balance. I am blessed to have an amazing support system in my husband and two boys, the rest of my family and friends.
For me, photography has been a powerful way to document my health journey and what I experience every day. It helps me see my progress, as well as setbacks in a cathartic way.
I am a registered nurse nationally certified in inpatient obstetrics. Unfortunately due to my illness, continuous surgeries and hospitalizations, I made the most difficult decision of my life and gave up the profession I worked so hard for and one that was a huge part of my identity. I am also an award-winning, internationally published photographer, focusing primarily on birth photography and self-portraiture. I found a new purpose, capturing laboring women and their deliveries combined both of my passions: childbirth and photography.

As a photographer, I believe that art enhances the well-being of individuals, society, and our environment and that artists have the power to heal, inspire, provoke, challenge, and offer hope. For me, photography has been a powerful way to document my health journey and what I experience every day. It helps me see my progress, as well as setbacks in a cathartic way. Photography allows people to see different perspectives and can be used as a tool for personal healing and positive change for many while nurturing creativity and self-expression.

My favorite quote is by the artist, Frida Kahlo. “At the end of the day, we can endure much more than we think we can.” I have definitely found this to be true and learned I am much more resilient than I ever thought I was. My illness has caused me to know myself better, which keeps my work honest and true. In the process, you truly meet yourself, which makes for better, more authentic work.
Contact Us

United Ostomy Associations of America
P.O. Box 2293
Biddeford, ME 04005-2293
Call us toll-free at: 1-800-826-0826.
Our Information Line hours are Monday-Friday, 9am to 3pm EST. If you have an emergency, please dial 911 or contact your local medical professional.
Please understand that UOAA is a private, nonprofit, advocacy and informational organization. We are not a medical facility and we do not have medical or legal professionals on staff. Therefore, UOAA does not provide Medical, Mental Health, Insurance or Legal Advice. Visit UOAA Virtual Ostomy Clinic provided by The Wound Company for non-emergency, virtual ostomy support.
Get Involved
UOAA is the leading organization proactively advocating on behalf of the ostomy community. Recognizing that we are always stronger together, we encourage everyone to get involved by joining our Advocacy Network. We’ve also created several Advocacy Tools and Resources to help you successfully advocate on behalf of the ostomy community to ensure every ostomate receives quality care.
Latest News:
 Steve Hubbard’s Ostomy and Crohn’s StoryApril 25, 2024 - 11:25 am
Steve Hubbard’s Ostomy and Crohn’s StoryApril 25, 2024 - 11:25 am Do you speak stoma?April 4, 2024 - 2:32 pm
Do you speak stoma?April 4, 2024 - 2:32 pm Why Larry David’s “Colostomy Bag” Curb episode is making me speak out about my ostomy after 48 yearsMarch 28, 2024 - 10:43 am
Why Larry David’s “Colostomy Bag” Curb episode is making me speak out about my ostomy after 48 yearsMarch 28, 2024 - 10:43 am Osmani Gonzalez’s StoryMarch 12, 2024 - 12:20 pm
Osmani Gonzalez’s StoryMarch 12, 2024 - 12:20 pm Ostomy Advocates Taking Action in Washington, DC for Digestive DiseasesMarch 8, 2024 - 4:14 pm
Ostomy Advocates Taking Action in Washington, DC for Digestive DiseasesMarch 8, 2024 - 4:14 pm

UOAA does not and shall not discriminate on the basis of race, color, religion (creed), gender, gender expression, age, national origin (ancestry), disability, marital status, sexual orientation, or military status, in any of its activities or operations.