Tag Archive for: ostomy
By Ellyn Mantell
It continues…the pandemic is rearing its ugly head and seems to be gaining strength once again, despite never universally weakening. Whereas we assumed by this time in the fall, we would be back to some sense of normalcy, we are, instead, buying jackets, shawls, gloves, and hats so we can eat outdoors and continue to safely socialize. Travel requires an army intelligence level approach including Ultra Violet wands, visors over masks, dozens of wipes, and gallons of hand sanitizer. Seeing family feels like a tease, since hugging and kissing are off-limits, with no change in sight. I could go on, but you know all of this, and more.
The one good thing that keeps me upbeat is the wonderful feeling of connecting with our support groups via Zoom. Ostomates still have concerns and needs, surgeries continue to happen, and new members need a safe place to begin their journey to their new normal. Even those of us who are comfortable and knowledgeable still need the same safe place to discuss concerns that continue to develop. And the ability to see familiar faces goes miles in feeling comfort.
I know from others who are doing virtual support group meetings that they, too, are feeling so much more secure in the roads they are traveling. Whether it is AA, or NA for addiction, or Alzheimer’s support for spouses or caregivers, cancer survivors, etc., people need to be able to talk and gain strength. Perhaps the ability to remain anonymous may be even more positive than in-person meetings.
Zoom and virtual meetings have been a lifesaver, and had we not been in this demanding situation, we may never have discovered that. I can still remember being asked to participate in a Zoom meeting a few years ago, and running as quickly as possible away from the involvement. It seemed so overwhelming and daunting. But necessity is truly the mother of invention, and I am eternally grateful that Zoom has made itself available for the masses.
Please consider reaching out to an ostomy support group via a computer or smartphone, if you are in need of…support. There is, undoubtedly, a group to help with almost every issue you may have. I believe I speak for those who facilitate when I say we care about you, want to help you, are likely to share your concerns and feelings, and most of all, are committed to you. I know that each ostomate who walks into my life represents an opportunity to help them look at their new life in a positive way, and with that in mind, our value is rather invaluable!
Ellyn Mantell is a UOAA advocate and Affiliated Support Group leader from New Jersey. You can follow her personal blog at morethanmyostomy
A Second Opinion Leads to a Life-Changing Ostomy
 In the spring of 2014, I had completed another colonoscopy for my ulcerative colitis. It was my fifteenth colonoscopy in twelve years and many prescriptions of drugs later to curtail the bleeding of the polyps in my intestine.
In the spring of 2014, I had completed another colonoscopy for my ulcerative colitis. It was my fifteenth colonoscopy in twelve years and many prescriptions of drugs later to curtail the bleeding of the polyps in my intestine.
I had a very productive career and life with a CPA practice for 34 years. In Grapevine, Texas I served on the school board and as a city council member, and was named “Citizen of the Year.” But bleeding and bathrooms were getting on my nerves, so I called the Mayo Clinic in Rochester, Minnesota, unbeknownst to my gastro doctor. I told them that I wanted another opinion.
After four days of extensive tests, discussions, colonoscopy, the doctors at Mayo concluded that the polyps were entirely too large to remove by minor surgery without bigger risks, and that removal of my large intestine was recommended. Cancer was discussed at length including risks and possibilities with large polyps and various medical unknowns involving my circumstances.
My large intestine was removed January 4, 2015. The surgery was in my home town and I had a great ostomy nurse that taught me all of the intricacies of the ostomy pouch and supplies. I returned to retirement life again here in the Mountains of Texas where it is cool in the summer and we return to Grapevine for the winter where we had our careers.
I am 76 today and walk with my dog 3 to 10 miles each day. I play golf anytime I can. I am very active in my small town and I play the organ at our church each Sunday. I am not overweight and enjoy eating most anything. I find it necessary to chew every piece of food very well. I avoid nuts, corn, kale, popcorn, and tough fruit skins.
I love life and I am so happy for the decisions I made.
Why they Happen and What to do
Elaine O’Rourke and Ostomy Nurse and Phoenix Magazine columnist Anita Prinz discuss ostomy leaks, reasons why they happen, what to do and how to help with skin breakdown. There is lots of valuable information in this interview for even those who have had their ostomies for many years. Elaine has had her ileostomy since 2005 due to Crohn’s disease and has had her fair share of leaks over the years until finding the right pouching system for her. If you are having persistent leaks then you should always consult with an ostomy nurse who can help find a solution for you.
You can find Elaine on Facebook and her “3 simple ways to overcome fears about your Ostomy” program at www.ElaineOrourke.com/ostomyprograms/
Saturday, October 3rd, 2020 marks the 10th anniversary of Ostomy Awareness Day. In partnership with United Ostomy Associations of America (UOAA), Hollister Incorporated is proud to stand with the entire ostomy community in celebration. Every ostomate has a voice worth hearing and we aim to embody ostomy confidence of our worldwide community with #OstomateVoices.
Spread Positivity and Share Your Voice

We’re connecting and empowering our worldwide ostomy community to share their own unique experiences—their challenges, their achievements and the joys of their daily lives. Share your words of encouragement that have helped you along your ostomy journey. Your story might help someone who might be struggling. Using your words, we’ll create a unique social card that you can share with your friends, family, and community. Share your voice here!
Join Us for a Virtual Cooking Class

Join us for a virtual cooking class on October 3rd with private chefs Ryan Van Voorhis, a fellow ostomate, and Seth Bradley of Nude Dude Food™, one of Chicago’s most sought after private dining and catering services. Register today to connect with others in the community and cook a delicious meal. Register today!
For more resources on nutrition with an ostomy, check out UOAA’s Food Chart or download the “Eating with an Ostomy” Nutrition Guide.
Show Off Your Stoma Sticker

Stoma stickers are a great way to raise awareness, start a conversation, or show support. Order your free Stoma Stickers in time for Ostomy Awareness Day, shipped anywhere in the US.
Share a photo or video of your Stoma Sticker on social media using #StomaSticker to be part of the conversation. Or show off your Stoma sticker while running in your virtual Run for Resilience Ostomy 5K and share how you celebrated #OstomyDay2020.
Share your #OstomateVoices and personalize your next Instagram or Facebook Stories with the Hollister “Ostomate Voices” digital stickers. It’s easy – search “Ostomate Voices” in the GIF library when creating a Story and you’ll find the whole collection, including a UOAA lifesaver and Stoma Sticker!
For more resources and interactive ways to get involved, visit Hollister.com/ostomyawareness.
Editor’s Note: this blog post was provided by Hollister Inc. the exclusive Diamond Sponsor of UOAA’s annual Run for Resilience Ostomy 5K events that benefit UOAA, a 501(c)(3) nonprofit organization.
 My journey with Short Bowel Syndrome (SBS) spans 61 years, and it has been full of twists and turns. I’ve often wished that I understood from the beginning exactly what it meant to have SBS – it is not temporary, rather it is chronic. That means it’s a lifelong condition, and it has frequently caused me to make adjustments to maintain my independence and lead a productive and meaningful life. Reaching independence and self-reliance took years of learning the importance of self-advocacy to get the information I needed from my healthcare providers, no matter how difficult it may have been to hear that information. Each symptom, diagnosis, ostomy and medical procedure that preceded my eventual SBS diagnosis posed new challenges. The more I knew about what lay ahead for me, the more I could take charge of my own life. As August marks SBS Awareness Month, I hope my experiences will help inform and inspire others living with this serious and chronic malabsorption disorder to speak up and ask for information and tips to help maintain as much independence as possible.
My journey with Short Bowel Syndrome (SBS) spans 61 years, and it has been full of twists and turns. I’ve often wished that I understood from the beginning exactly what it meant to have SBS – it is not temporary, rather it is chronic. That means it’s a lifelong condition, and it has frequently caused me to make adjustments to maintain my independence and lead a productive and meaningful life. Reaching independence and self-reliance took years of learning the importance of self-advocacy to get the information I needed from my healthcare providers, no matter how difficult it may have been to hear that information. Each symptom, diagnosis, ostomy and medical procedure that preceded my eventual SBS diagnosis posed new challenges. The more I knew about what lay ahead for me, the more I could take charge of my own life. As August marks SBS Awareness Month, I hope my experiences will help inform and inspire others living with this serious and chronic malabsorption disorder to speak up and ask for information and tips to help maintain as much independence as possible.
A very long time ago, before cellphones, DVD players, home computers, microwaves and color TV, I was born in New Jersey in February 1959. I was a very “clean” baby, with no dirty diapers, which soon raised concern among the medical professionals who started me on enemas and laxatives. I ate very little and projectile vomited most of what I did eat. My mother continuously tried to find out what was wrong with me. Despite many doctors advising her that it was a discipline issue, no diagnosis made sense. None of their theories panned out. Nothing worked. And so began a long journey of wishing we had known what I was living with much earlier on.
In the summer of 1963, my mother, in her desperation, called the White House, spoke to the switchboard operator and requested the name of the Kennedy children’s pediatrician. She then made an appointment with the chief of pediatric surgery. The doctors conducted multiple tests, but unfortunately, I was discharged before the test results were back as the hospital was dealing with another emergency patient! Consequently, my mother did not receive the results, and we left wishing we had more answers.
It took three more years, another hospitalization and my first surgery for a doctor to request those records and discover I should have been diagnosed with a rare, congenital condition called Hirschsprung’s disease back in 1963. Back then, my family and I didn’t know that this diagnosis would increase the likelihood of future gastrointestinal procedures and diagnoses, including SBS. In fact, after that first surgery, my doctors told me I would be fine. Yet, I developed a fistula and the treatment/surgery for that left me with an ostomy. It closed within a year, and my parents were told yet again that I was fine, and we had learned all we needed to know.
Throughout my childhood, I continued to experience episodes of vomiting and few bowel movements, which left me very thin. To stop the vomiting, I had a laparoscopic procedure as a young adult, which I hoped would be the last of my surgeries – if only I had known what lay ahead. My surgeries did not stop there as I had hoped, and I had a second and third ostomy. In 2002, I was placed on total parenteral nutrition (TPN) for the first time. At that time, I was only receiving TPN during my stay in the hospital while recovering from surgery. My body had tried to cover up the symptoms of malabsorption for more than forty years, and I was now seeing the effects of my severe nutritional deficits. I would return to needing TPN periodically over the next two decades.
In graduate school, I met my husband, and we now share a wonderfully supportive family. When we wanted to start a family, there were some severe issues with my pregnancies. My firstborn was delivered via emergency caesarean because I couldn’t stop vomiting. I was hospitalized seven times during my second pregnancy. And then when I finally went into labor, my blood pressure dropped drastically throughout the delivery. I’m happy to say that despite their dramatic entrances, my daughters are happy, healthy and successful – both are biomedical engineers, and one is also a doctor.
In April 2006, I participated in a colonic motility study, and what I’d learned in pieces over the years was finally confirmed: my colon was functionally deficient.  Six years later, I found myself unable to eat due to severe abdominal pains and a pseudo-obstruction and was put back on TPN. I feared this would prevent me from traveling on a three-week family trip to Australia, but my husband and daughters learned how to properly store, prepare and administer my TPN infusions, so we could still travel. I am so grateful to have been able to enjoy that trip with my family despite my TPN, ostomy and needing to use a catheter. I would encourage families and caregivers of people living with ostomies and/or SBS to take every opportunity to promote their self-care and independence as much as possible. For me, traveling with my family is important. Learning how to pack and plan our trips in ways that help me maintain my independence has made a big difference.
Six years later, I found myself unable to eat due to severe abdominal pains and a pseudo-obstruction and was put back on TPN. I feared this would prevent me from traveling on a three-week family trip to Australia, but my husband and daughters learned how to properly store, prepare and administer my TPN infusions, so we could still travel. I am so grateful to have been able to enjoy that trip with my family despite my TPN, ostomy and needing to use a catheter. I would encourage families and caregivers of people living with ostomies and/or SBS to take every opportunity to promote their self-care and independence as much as possible. For me, traveling with my family is important. Learning how to pack and plan our trips in ways that help me maintain my independence has made a big difference.
In August 2013, I was once again faced with just how much I didn’t know about my condition when I was officially diagnosed with SBS. My doctor explained that, rather than solely due to the length of my bowel, my SBS diagnosis was based on my clinical symptoms. My intestines could not sufficiently absorb the nutrients my body needed, leading to malnutrition and dehydration. To maintain nutrition, I continued on TPN.
After finally reaching 145 pounds in September 2019, I was told to discontinue TPN. With SBS, however, I do not know how long this reprieve will last, and these unknowns are important motivators for me to self-advocate when it comes to talking to my healthcare providers. As much as possible, I think healthcare providers should be upfront about the ramifications of living with SBS to fill the gaps in understanding disease management. For me, I spent a lot of time learning as I went along, and my hope is that by sharing my experiences, I can encourage others to ask the tough questions every step of the way.
I am thankful my husband and daughters have always been there for me, helping me emotionally at every doctor’s visit. My husband especially helps me get through each learning curve and the occasional late-night clean-up from messy ostomy accidents. I even have a service dog who carries my medicine for me wherever I go – I consider him my personal ambulance. Without this wonderful support around me, my life would be much more complicated.
That support has helped me take an active role in advocating for myself and others with ostomies, feeding tubes and other GI issues. Each condition differs in how they affect us physically, yet many of us share common concerns. Though people like me may appear healthy on the outside, I want to increase awareness that SBS can be a hidden illness requiring a lot of medical maintenance, sometimes including an ostomy and feeding apparatus. I want to support those like me who also may feel overlooked. Because of that, I started a support group that focuses on ways to continue living our lives, discussing everything from travel to preparing for emergencies. I also advocate on the national level, attending National Institutes of Health conferences in Washington, D.C. I would encourage patients and caregivers to attend local support groups as well as regional and national conferences to meet other people with SBS to share experiences and tips.
These opportunities to connect with the community of patients and caregivers managing GI conditions help to remind me I am not alone. Our individual journeys to SBS diagnosis may involve varied GI conditions and symptoms, and it can feel challenging to find others who share our experience. Sometimes our family and friends forget that we are not quite as physically strong or have stamina unless we mentally prepare ourselves for individual occasions. But in our shared SBS community, we can truly feel related to, supported and understood. I may not have had all the answers along the way, but with support and community I don’t have to dwell on what I wish I had known. I can simply live and learn through each moment.
To join the community and learn more about others living with Short Bowel Syndrome (SBS), visit https://www.facebook.com/TakedaSBS. You can also engage with #shortbowelsyndrome on social channels, especially during the month of August, which is SBS Awareness Month.
This article was created and sponsored by Takeda.
Editor’s Note: This educational article is from one of our digital sponsors, Takeda. Sponsor support along with donations from our readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.
Having an ostomy should not prevent you from swimming. Below are some helpful tips to get you feeling confident in the water, whether it’s in your own backyard pool or at a beach.
- You can swim or be in the water while wearing your pouching system. Remember, your pouching system is water-resistant and is designed not to leak with the proper seal. Water will not harm or enter your stoma.
- Prior to swimming, make sure your seal is secure.
- Empty your pouch before swimming. Also, ensure your wafer has been on for at least an hour prior to getting wet. If you are nervous about output, eat a few hours before jumping in.
- If you use a filtered pouch, use a filter cover sticker on your deodorizing filter to prevent water from entering the pouch. You can remove the cover once you are dry.
- Wear what makes you feel the most comfortable. Swimming with an ostomy should be fun and worry-free regardless of what you’re wearing. Shop with confidence knowing there are so many options that could work for you.
- Always carry extra supplies in case you are somewhere where supplies may not be available.
- For extra peace of mind, use barrier strips if you will be swimming for an extended time.
me+ Team Member Tip: “I tell people who are scared to swim with an ostomy to spend a few hours in the tub on a lazy day. If your pouching system holds up to that, then the pool should be a breeze.” ~Sarah B.
Editor’s note: This article is from one of our digital sponsors, ConvaTec. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.
A patient who did not know what to expect walks you through the process (with photos)
By AnneMarie Finn
According to UOAA information on this website, a urostomy is “a surgically created opening in the abdominal wall through which urine passes. A urostomy may be performed when the bladder is either not functioning or has to be removed. There are several different types of surgeries, but the most common are ileal conduit and colonic conduit. Reasons for surgery include bladder cancer, spinal cord injuries, malfunction such as chronic infection of the bladder and birth defects such as spina bifida.” Great definition, but what does it mean? When I was told I would need a radical cystectomy, leading to an ileal conduit I had no clue. The following is my experience.
Because of bladder cancer, my bladder needed to be removed and a new way to pass urine created. Due to the location of the tumor, my urethra was also removed so my surgeon and I settled on an ileal conduit, a conventional urostomy. It is called ileal conduit because a piece of the ileum, or small bowel, is used to make a passage for urine to go from the kidneys and ureters out of the body. The other end is brought out through a hole in the abdomen where urine exits through a stoma (more on that shortly). It is known as an incontinent urinary diversion because you cannot control the urine. As a result, a collection bag or pouch hangs from your abdomen to catch the urine. The pouch is not visible as it is worn under your clothes. Still not clear? It wasn’t for me either.

A couple of days before surgery, I met with an ostomy nurse at the hospital where I would be receiving my surgery. She marked where the stoma would be placed. She saw how I wore my pants. She had me sit, stand, lay down, and bend over, She drew a mark with a marker about 2.5 inches to the right and 3 inches down from my navel and covered it with a waterproof dressing. This would guide the surgeon as to the optimal spot to place the stoma. The surgeon had the ultimate call on where the stoma went, depending on the surgery itself. I also met with a nurse for a pre-op appointment. They went through the typical exam and then explained the ERAS protocol to me. ERAS, Enhanced Recovery After Surgery, is used at my hospital for radical cystectomies. They no longer use a bowel prep. You drink a high carbohydrate drink in the hours prior to your surgery. They get you up walking and feed you by the day after surgery. The goal is to keep your bowels working. This reduces the length of hospital stay and the number of complications.
This is major surgery. It is considered one of the most complex cancer surgeries performed. My surgery took 7 hours. They removed the bladder, urethra, uterus, cervix, fallopian tubes, an ovary, and some lymph nodes. When I woke up, I had a bag, a large incision with more than 30 staples and a Jackson Pratt (JP) drain on my abdomen. I also had intermittent pneumatic compression (IPC) devices on my legs, my spa legs. Blood clots are a common side effect of a radical cystectomy. Because of that, I also received daily prophylaxis blood thinner shots in my belly for 30 days. I was not in a great deal of pain which was easily managed with Tylenol. I was definitely weak, but otherwise ok. I went home in 4 days, on my own with my urostomy.
I was not in a great deal of pain which was easily managed with Tylenol. I was definitely weak, but otherwise ok. I went home in 4 days, on my own with my urostomy.
The stoma is the badge of the urostomy. My stoma is about one inch in diameter. It is pretty round, It sticks out. It sometimes moves in and out. You can’t feel it. It has been described as looking like a rosebud. It is red. This is where the urine exits the body. You have no control over it. Sometimes it will also expel mucus. Some people name them. I did.
 Rudolph, my red, round stoma
Rudolph, my red, round stoma
You use a urine collection pouch, or bag, to catch the urine. The hospital will send you home with some so you do not need to have them on hand before you get home. There are many different brands. In fact, until I found what worked best for me, I tried most of them. My pouch is about 8 inches long, 6-7 inches wide and has a 1-2 inch closable spout on the bottom. It also is a deep convex bag as my stoma does not stick out very far and it helps protect my skin. I prefer the clear bag so I can see the stoma and center it when I put it on. There are both one and two-piece bags. I have used both. One-piece pouches have the bag and a skin barrier attached. The skin barrier has adhesive, also called a flange or wafer, that sticks to your skin. There is a hole that goes over the stoma. Some are pre-cut, some are not. If not, you must cut a hole slightly bigger than your stoma before putting it on. There are also two-piece systems. The bags are separate from the skin barrier. They are attached by a Tupperware-like seal. You can leave the skin barrier on and take off the pouch.

Front and back of 1 piece, deep convex pouch
I change my pouch every 3 days. I like to remove the old pouch and take a shower with it off. I feel so free. To remove, I use an adhesive removal spray and wipes to clean the skin. I shower and wash the area around the stoma with soap and dandruff shampoo, which contains Zinc. Some people wash with a vinegar and water combo. If I change without showering, I just use plain water to rinse. After showering, I use a hairdryer on the lowest setting to dry the skin around the stoma so the wafer sticks to it. Drying your skin is important. I have some skin issues so I also use a skin barrier protective sheet, that I cut a hole to match the opening of the wafer, and a cohesive seal.
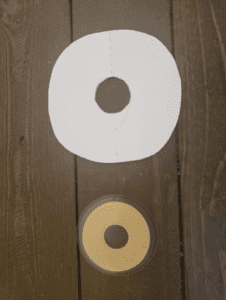
Protective Sheet with hole cut out and Cohesive Seal
Some people use powders, paste, barrier wipes, etc. I do not. It took a lot of trial and error to find what worked best for me. You need to find what works for you. One of the best ways to do this is to work with an ostomy nurse. They can help you navigate ordering and finding the best system for you.
At night, I use the urinary drainage bag they sent me home with from the hospital. For me, it works the best. There are several brands of night bags and even jugs. I put it on the floor next to my bed inside of a small wastebasket. This has been key as the drain has opened (or been left open) and the wastebasket collected the urine, preventing a rug catastrophe. I am a very active sleeper and I am not really hindered too much from my bag. I am able to sleep on my back, sides, and stomach. Don’t be afraid to sleep. People add their own tubing and tube placement strategies. Use whatever works for you. I also highly recommend a waterproof mattress pad. Mattresses are expensive. I also use the night drainage bag on long car trips. I don’t have to stop and use those disgusting public toilets. I even used it during the Avengers finale. I was probably the only person in the theater who did not have to get up to use the facilities during the movie! People were actually jealous.
 Night Drainage Pouch
Night Drainage Pouch
I honestly can’t even feel my pouch. I empty it every 1-2 hours, depending on how much I drink. Sometimes there is a “ghost” feeling where my bladder used to be making it feel like I have to pee. Ah, the good old days. It is actually a weird sensation drinking a lot and not feeling like I have to go. The bag is not noticeable under my clothes. I really do wear what I wore before surgery: jeans, sheath dresses, shorts, and bathing suits. I am still sexually active. Having gone through this experience with my wonderful caregiver, my husband, has brought us closer. Most importantly, I am cancer-free.
 Finding Hope in the Stories of Others
Finding Hope in the Stories of Others
By Scott Steehn
All stories have a beginning, and mine is no different. It started on a cold, slate-colored February day in Erie, Pennsylvania in 1992. I was a successful standup comic who had headlined clubs and theaters in all 50 states and seven foreign countries. I was recently engaged to my soulmate, and we were making plans for a big October wedding. I was just finishing up a great week at a terrific comedy club in Erie and, as I prepared for my two shows on Saturday night, I felt like everything couldn’t have been going any better. But, in just 12 hours, none of those things would matter.
It started when I was onstage during the first show. I began having abdominal pain on my left, lower side. It wasn’t a huge pain and mainly felt like a had a fairly intense need to move my bowels. I finished up my show and made a beeline to the restroom. And…nothing happened. Nothing at all. The NEED was still there, and, in fact, it was getting worse. I, of course, had been constipated before, but this felt somehow…different.
I did my second show, but the pain was now almost unbearable. I headed back to my hotel, stopping only at a drugstore to pick up a laxative. I had convinced myself it was just constipation and had even assigned the blame to the shrimp dinner I’d had the night before. “Fresh Shrimp” in February…in Erie?! What did I expect to happen?
I took the laxative. And I waited. And tried. And waited some more. And then the pain got bad. Real bad. I could barely walk and couldn’t move without intense pain shooting out from my left side. Now I had a new theory. Burst appendix. This was before the days of Web MD, and I was limited to only what my imagination could conjure to freak myself out. So, not wanting to die a ridiculous death in the Erie Hilton, I called a taxi and headed to the hospital.
They got me into an exam room in short order. The doctor examined me and, taking advantage of his fancy medical degree, immediately eliminated appendicitis. So much for that. He then told me he had an idea what it was but wanted an MRI to confirm the results. A quick trip through the “donut of doom” confirmed his initial diagnosis. It was something called diverticulitis. He explained how we all have small abscesses in the colon and how they usually don’t cause any problems. Sometimes, however, those abscesses become infected. It causes horrible pain and constipation, and once it gets this bad, it has to be treated with antibiotics and mass quantities of fluids. I spent a painful week in the hospital and was discharged with very specific instructions on how to adjust my diet and lifestyle to prevent a recurrence. I thanked all the staff for the great job they did, signed some papers, checked out…and promptly ignored his instructions for the next 20 years.
Christmas Eve, 2012. My wife has had enough. The final straw came when I was unable to make it upstairs for the family gift exchange. As soon as it was over, she came down and told me we were going to head to the emergency room. I didn’t have the energy to argue. Plus, I knew she was right. I’d been feeling terrible for almost three years. Something was definitely not right. It seemed like it emanated from the “diverticulitis spot” that I had become intimately familiar with due to the flare-ups I suffered through two or three times a year. The only confusing part was I had undergone a colonoscopy six months prior and had received a clean bill of health. Only much later did I learn that I had received a negligent result. My doctors all agreed- there was no way my problem could have been missed.
I should have known I was in trouble when, after the emergency room doc saw me initially, he asked me if I’d like anything for pain. I jokingly said, “Sure, how about some morphine?” He immediately replied, “Okay, we’ll get that going for you.” Uh oh. A little later he told me I had a blockage that had been caused by a buildup of scar tissue from the repeated flare-ups of diverticulitis. They needed to get rid of the infection and then remove the two damaged sections of bowel. Surgery was scheduled for New Year’s Eve. Merry Christmas and Happy freaking New Year!
I spent the next week in a morphine haze. I met my surgeon, a brilliant young lady who looked impossibly young for someone with that much schooling. She explained that they were hoping to remove the damaged sections laparoscopically. It was a relatively simple procedure that would require a couple of days of recovery in the hospital, a week or two at home, and then back to my normal life. The alternative would be invasive surgery, much longer recovery time, and, while the healing took place, I would need to have a colostomy. Due in part to my opiate fog and also due to my refusal to accept reality, I was 100% convinced everything would be done laparoscopically. No worries.
The first thing I noticed when I came to was something in my throat. Something huge and foreign. As my world blinked into focus, the nurse was there to explain to me that the damage was much worse than they had anticipated. Full surgery had been performed and I was going to be in the hospital for a while. The drugs were very helpful in allowing me to deny exactly what exactly that meant. I was much more concerned with getting the tube out of my throat and the catheter out of the other end. That cavalier attitude about my situation would soon change.
The nurses and staff were great. They changed my colostomy bag for me and allowed me to STILL not grasp my situation. That all changed when I met the ostomy nurse. She was tasked with teaching me the intricacies of daily life with a colostomy. Reality came crashing through the door when I spent 30 minutes hiding in the restroom in tears unable to change my bag. I can’t do this! This isn’t fair! (Conveniently forgetting the 20 years I had spent ignoring my doctor’s orders) Gathering myself, I sucked it up, and FINALLY was able to do it on my own. I was discharged and sent home to recuperate and heal for 30 days before heading back to the hospital for takedown surgery.
I’d like to tell you a story about how well I adjusted. About how I was brave. About how I was thankful to be alive. About how I now appreciated my friends and family even more. About how I would now refused to take all the beauty of life for granted. That’s the story I’d like to tell. But I can’t. It would be a lie. Even though none of you know me, I promised myself I would be 100% honest about my journey. Warts and all. So here goes.
It was awful. I hated every minute of it. I thought having a colostomy was gross. And hard. Life wasn’t fair. NOTHING was fair. I can’t do this. There were the usual indignities. Accidents. Broken seals. Excess gas. I was in hell. Never for one moment did I think how my situation affected those around me. How my actions and attitude affected my family, and, my wife in particular, who only wanted me to get better and get back to being the man she married. As an added bonus, I was also taking 12 Oxycodone a day for pain, and, rightly suspected, now had a raging opioid addiction. My day consisted of sleeping, crying, bitching at my family, thinking about death, and dealing with my new, hated, appendage. Day after day. Rinse, lather, repeat.
Then, one day while noodling around on the internet, I found UOAA. I started reading about my condition. And I started reading other people’s stories. I found out just how many dealt with this particular challenge. I was stunned. And the more stories I read, the more my respect grew. People who had to deal with this for years. For decades. Tears streamed down my face as I read their stories. I’d love to tell you everything changed that day. How my attitude changed overnight and how I became Mr. Positivity. Alas, it wasn’t that simple.
What DID happen, is I became embarrassed about my actions. I had always prided myself on being a tough guy who dealt with problems head-on. The more I read on ostomy.org, the more I knew this was a lie.
Every day I read the stories of real heroes. Men and women who possessed the biggest superpower of all, the ability to live a normal life despite adversity that was currently bringing me to my knees. To say they inspired me, would be an understatement. Closer to the truth would be, they saved my life.
They gave me practical advice, “insider tips” on everything from bathing to sex, and something I hadn’t felt in a long time. They gave me hope. I never posted on the UOAA discussion board. Hell, I don’t think I even registered. Due to my “temporary” status, I really didn’t think anyone wanted to hear my whining. If everything went well, my life would go back to “normal,” while these people would continue to lead quietly heroic lives day after day, year after year. I didn’t feel worthy. And I still don’t.
That’s my story. Sure, there’s more, including an unsuccessful takedown, massive infection, emergency surgery, and an ileostomy for a few more months. There was a wound vac, and an in-home nurse to change my dressing daily. And, of course, after 6 ½ months of daily opioid use, I still had to deal with that King Kong-sized habit. Yet, in the end, I was okay. It probably took almost two years to feel like me again. And even that isn’t completely accurate.
I recovered, I felt better physically, but “myself” was different. I was more appreciative, more humble, and more thankful. I was well, but I’d never be the same.
So, thanks for reading. Thanks to Ed Pfueller for giving me an opportunity to share my story. Thanks to the whole team at UOAA and, for that matter, all of the sites designed to educate, inform, and help everyone on this particular journey. Lastly, more thanks than I could ever express to all the men and women who bravely shared their stories through blogs and forums. Thanks for your bravery. Thanks for your humor. And thanks for giving me the courage to understand and accept my condition with, what I hope, was grace and determination that would make you all proud. God bless each and every one of you and may your lives be full of the joy and love that you so richly deserve. I am forever in your debt.
It’s Ivan’s 4th Birthday!
Four years ago today my amazing doctors, Dr. Leslie Demars and Dr. Joga Ivatury removed a huge tumor out of my pelvis and I woke up ALIVE and in a colostomy which I named (Ivan) after Dr. Ivatury, for life.
The first thing I asked Dr. Ivatury when I woke up was “did we get the f#@%r?” He smiled and smiled and said yes.
The next thing I asked was “am I in a bag?” He reluctantly said “yes.” My reaction? “Ok now let’s get me out of here so we can go to California.” I was working on a Tyra Banks product line at the time and did not want to miss the opportunity.
I was not always so positive. When I found out I had cancer in 2015 and would possibly be in a colostomy bag for life, I was devastated, to the point where I told my doctor “do NOT put me in a bag” so many times that he had to yell at me and say I have been up nights thinking about your surgery, I have no intention of putting you in a bag HOWEVER my job is to SAVE YOUR LIFE. So well, he was right.
I had such a different view on life when I woke up. God left me here to do some work and I was not going to let HIM down by playing small. I was going to live my life HUGE and give back to this world as much as I can.
I did allow myself to have strong feelings and concerns. “What if it smells, or makes noises or someone bumps it?” I would cry after cancer, but life was not over yet. What am I supposed to learn from this lesson and from what I am going through? It took me a lot of work to get to be okay. We got this one life.
I got up and forced myself to get out anyway. It helped so much that my kids, parents, and sister along with my husband and friends were supportive of me along the way.
I wanted to get back to doing the things I had enjoyed before cancer. One love was competing in Fitness America and WBFF shows in 2010 and 2011, where I placed in the top five in one of the shows I did. I knew I needed to love my body again and decided to tell the world in a live video to let people know to love the body you were given.

LeeAnne Hayden competes with her colostomy pouch and all at the 2017 America Fitness weekend in Las Vegas.
I was talking with my husband and friends and said I think I want to compete with “Ivan.” The second it came out of my mouth everyone was so supportive. I was sponsored for my training, plane, suit, costume, all of it. When I got there after months of training I almost didn’t want to do it. However, I knew I couldn’t let my fear stop me, I had to show everyone what I preached. The costume was great. It was a pair of wings that I could open and expand. I was shaking when I took my first steps out on that stage, I took a deep breath and opened the wings, hit my pose and completely teared up when everyone in the audience stood up clapping, screaming and some of them were crying. (Gosh I am starting to cry writing this) It was the most surreal moment ever. I felt amazing and supported and forgot I even had Ivan while I hit all my posing and walked off the stage to my friends in the back screaming and hugging me. It is a moment I will never forget.
There is such a stigma to ostomies, I have heard stories of how people have given up their lives because they didn’t want to be in one. I think we all need to be more vocal about it. So many more people could be saved. Thank you to UOAA for what you do with ostomy awareness!
That’s the way I’ve spent these last four years and I can’t wait to see where my life goes from here! I want to bring everything I have personally been through to all of you so that you may grow and live the life you want and deserve! Huge thank you to my wonderful doctors, my amazing family, my friends, all of you, and especially to GOD for allowing me to remain.
Whatever you want to do in life hope you run for it.
LeeAnne Hayden blogs about her life here and produces the LeeAnne in the City Podcast.
Contact Us

United Ostomy Associations of America
P.O. Box 2293
Biddeford, ME 04005-2293
Call us toll-free at: 1-800-826-0826.
Our Information Line hours are Monday-Friday, 9am to 3pm EST. If you have an emergency, please dial 911 or contact your local medical professional.
Please understand that UOAA is a private, nonprofit, advocacy and informational organization. We are not a medical facility and we do not have medical or legal professionals on staff. Therefore, UOAA does not provide Medical, Mental Health, Insurance or Legal Advice. Visit UOAA Virtual Ostomy Clinic provided by The Wound Company for non-emergency, virtual ostomy support.
Get Involved
UOAA is the leading organization proactively advocating on behalf of the ostomy community. Recognizing that we are always stronger together, we encourage everyone to get involved by joining our Advocacy Network. We’ve also created several Advocacy Tools and Resources to help you successfully advocate on behalf of the ostomy community to ensure every ostomate receives quality care.
Latest News:
 Do you speak stoma?April 4, 2024 - 2:32 pm
Do you speak stoma?April 4, 2024 - 2:32 pm Why Larry David’s “Colostomy Bag” Curb episode is making me speak out about my ostomy after 48 yearsMarch 28, 2024 - 10:43 am
Why Larry David’s “Colostomy Bag” Curb episode is making me speak out about my ostomy after 48 yearsMarch 28, 2024 - 10:43 am Osmani Gonzalez’s StoryMarch 12, 2024 - 12:20 pm
Osmani Gonzalez’s StoryMarch 12, 2024 - 12:20 pm Ostomy Advocates Taking Action in Washington, DC for Digestive DiseasesMarch 8, 2024 - 4:14 pm
Ostomy Advocates Taking Action in Washington, DC for Digestive DiseasesMarch 8, 2024 - 4:14 pm Sexual well-being and intimacy after ostomy surgeryFebruary 22, 2024 - 4:02 pm
Sexual well-being and intimacy after ostomy surgeryFebruary 22, 2024 - 4:02 pm

UOAA does not and shall not discriminate on the basis of race, color, religion (creed), gender, gender expression, age, national origin (ancestry), disability, marital status, sexual orientation, or military status, in any of its activities or operations.
