Every Individual is Unique so Don’t Put Restrictions on Yourself Based on Others
By Lisa Febre
The morning after my colectomy, the first question I had for my surgeon was “can I still do yoga?” My surgeon had a good-natured and amused response: “Please give yourself two weeks to recover from this surgery, and then you can do all the yoga you want.” He also told me that with my specific colostomy, in two weeks I could get back to my regular diet with no restrictions. (I’ve since learned those with an ileostomy have different considerations.)
Sure enough, two weeks later, once I was sufficiently recovered, I was living out his predictions. I was back on the yoga mat, twisting myself into pretzels, lifting into tricky arm balances, and standing on my head. I was outdoors hiking and running. For the first week after surgery, I was following a soft-solids diet, and by the second week I was eating whatever I wanted. By the end of the month, I was even eating Reuben sandwiches with sauerkraut!
I knew no boundaries because I had none.
It wasn’t until I joined a support group on social media that I noticed people were questioning things I was taking for granted like taking a shower, exercising, wearing pants, and eating vegetables. Are there eating restrictions for ostomates? Was it possible some people were told they could not exercise with their ostomy? The answer is …yes… ish.
Showering with an Ostomy
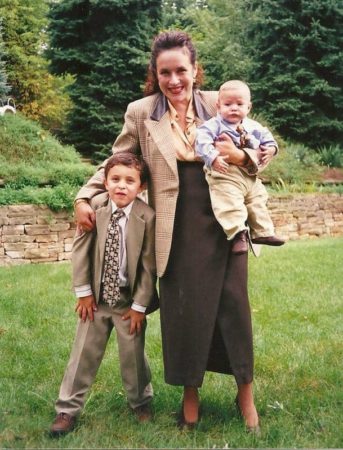
I was given a temporary colostomy in December 2021 when I was diagnosed with Stage-4c Colon Cancer (at the age of 47). There is no way around it: this is a big shock to the body and the mind. But the only thing I could think about was getting into the shower and washing off the five days’ worth of sweat and grime that had accumulated on my body during my hospital stay. I stripped down, my new Hollister 2-piece system hanging off of me and stepped into the shower. I didn’t think about the bag at all, I just showered like I normally did. When I was done, I dried myself and the bag off with a towel, and… that was it. I did this every single day without a second thought.
I would laugh at myself and say: it’s just poop, it’s not nuclear waste!
Weeks later, I was surprised to learn people commenting online were wrapping up their colostomy bags with layers of plastic wrap and were trying desperately to keep their abdomens out of the water. Wait… are we not supposed to get the bags wet? That didn’t sound right to me. The barrier has to be taken off with adhesive removal wipes or sprays, and even then, it can be difficult to separate it from your skin. The durable plastic receptacle bag is meant to hold all kinds of bodily fluids, it seems obvious that it should be able to handle a little soap and water. The customer service reps at both Hollister and Coloplast concurred: they specifically told me that their products are meant to be used while showering, bathing, and even swimming, with no extra accessories. Again, because no one told me I couldn’t, I was already doing these things. It was heartbreaking to see so many of my fellow ostomates avoiding basic hygiene for fear of doing it with the bag on.
It seems like the solution might be to shower without the appliance. There tends to be even more fear surrounding this practice of naked showers. Again, this was something that I had already done without asking for permission. One day I was changing my appliance, decided it would be a great time to shower, and just jumped in. The soap on my newly exposed skin felt fantastic, my stoma looked to be enjoying the water running down my belly. Naked showers were soothing and necessary for my peace of mind. I always felt the cleanest when I showered without my appliance. The skin under the barrier stayed healthy and the adhesives worked much better. Always close at hand was a disposable plastic cup filled 1/4 up with water which I used to catch any “visitors” that might erupt from my exposed stoma during my shower. I would laugh at myself and say: it’s just poop, it’s not nuclear waste!
 Exercising with an Ostomy
Exercising with an Ostomy
This is something you absolutely must talk to your doctor about. I can’t give you proper advice since everyone has a different risk value for a parastomal hernia (that’s when your intestines try to push their way through the incision around the stoma). Although 50% of people with a stoma will get a parastomal hernia, that doesn’t mean you are going to get one. Your surgeon will assess your risk. I had almost no risk of one of these hernias because I was fit and active before the surgery; there was a low likelihood that my incision site would fail while I had the stoma. I was told I could begin exercising again 2 weeks post-op. Alternately, when I had my reversal surgery 10 months later, my surgeon said there is a slightly higher risk of a hernia at the closure site and wanted me to wait 8 weeks before lifting anything over 10 pounds, and that included doing yoga.
Even within one person, my risks were different for each surgery. This is why you have to have a clear assessment from your doctor and follow their directions. Some people may still develop a hernia despite following their surgeon’s directions. It’s important to question and clarify, but ultimately listen to your doctor– and not just people online, this gives you the best chance for success.
Dressing with an Ostomy
This is a tricky one for ostomates because everyone’s stoma is in a slightly different spot. I was able to wear jeans and form-fitting clothing because the location of my stoma made that possible. Someone else may have their stoma exactly where the rigid waistband of their favorite jeans falls, which can be an issue. Your clothing isn’t necessarily going to hurt the stoma, but you do need to save room for when your stoma has output. For some, tight-fitting clothing can restrict the bag, forcing the output backward toward your skin and under the barrier.
Dressing is definitely not a one-size-fits-all situation, so unfortunately no one can really give someone else game-changing advice. Be ready to experiment, but always wear clothing that makes you feel good. It was important to me to wear jeans, so I bought new jeans with a lower waistband that fell just under my stoma. Many other women invest in maternity pants. But I never left the house feeling frumpy. My colostomy was not in charge of my fashion sense, I was!
Eating with an Ostomy
Everyone has a unique reason for having an ostomy. In my case, I had my colostomy because of cancer; I had no pre-existing intestinal issues or dietary restrictions. If you are like me and could eat whatever you wanted before, chances are high that your doctor will tell you you can go back to that way of eating after your surgery. But some people, who come to a colostomy or ileostomy through ulcerative colitis or Crohn’s disease (or other gastrointestinal disease), may already have restrictions that they still need to take into consideration. An ostomy does not always magically erase your special diet for your IBD.
The general rule is however you ate before your colostomy is how you can eat now.
It does not rule you; it is not the most important thing about you, and it does not define your life.
I am vegan and I had no trouble eating any vegetables with my colostomy. UOAA’s trusted Eating with an Ostomy Guide provides info including a standard chart of foods to avoid at first with an ileostomy or colostomy – whether that is because they create stinky output, excess gas, diarrhea, constipation, or could cause blockages. Speak with your doctor and surgeon if you are unsure how to handle building your new diet. If you’re introducing new vegetables (or any kind of food) into your post-colostomy diet, just try a little bit and see what happens! If your doctor says it’s ok, don’t be afraid to try eating the old things you love, and maybe be inspired to try some new things as well. A good practice for all is to chew thoroughly and stay hydrated.
Stay Positive with an Ostomy

 Some people wonder how they can ever find something positive in something so scary as an ostomy, but it can be done. You don’t need to do it in big
Some people wonder how they can ever find something positive in something so scary as an ostomy, but it can be done. You don’t need to do it in big  grand gestures or sweeping alterations in your character. Just try one little switch when the opportunity comes up. It isn’t about skipping down the street singing the praises of your ostomy, it’s about finding moments when you can see the silver lining. I thought it was sort of fun to have something so unique on my body. Very few people ever get to have this close a relationship with their intestines, so instead of feeling sorry for myself, I decided to call myself “lucky” for learning so much about how my digestive tract works.
grand gestures or sweeping alterations in your character. Just try one little switch when the opportunity comes up. It isn’t about skipping down the street singing the praises of your ostomy, it’s about finding moments when you can see the silver lining. I thought it was sort of fun to have something so unique on my body. Very few people ever get to have this close a relationship with their intestines, so instead of feeling sorry for myself, I decided to call myself “lucky” for learning so much about how my digestive tract works.
Maybe most important of all, my ostomy led me to a UOAA support group where I met some wonderful people. I have made new friends who I would never have met without my ostomy. That is something to be very thankful for.
Spend some time every day when you force yourself to not think about your ostomy. Even if it’s just 20 seconds, it is important to learn to push this thing into the background of your life. It does not rule you; it is not the most important thing about you, and it does not define your life. Stay Positive! One day, one hour, sometimes one minute at a time, but you can do this.
Learn to Take Care of Your Ostomy
Our emotional recovery depends on regaining independence. I was only 47 when I received my ostomy. I am too young to rely on others to take care of me. I laughed when the home health aide arrived and started treating me like I was 80. I was not going to lie down and become helpless. I was going to be an active participant in my own health and recovery.
Learning how to care for yourself makes you feel like a Superhero!
If you suddenly find yourself having to depend on someone else to maintain your appliance, you will feel even more out of control and worried that something might go wrong. Believe me: something will go wrong — leaks happen to the best of us, and at the most unexpected times. If you have to wait until your nurse can come to your house, or until your partner gets home from work, you will feel more helpless with each passing day. Paranoid that something terrible will happen if you get a leak while you’re alone, you may not leave the house to run errands, you may say no to social gatherings, and you may not want to go back to work.
Learning how to care for yourself makes you feel like a Superhero! I had a cool little zipper bag that fit in my purse containing a precut barrier, 2 extra bags, 2-3 adhesive remover wipes, 2-3 skin prep wipes, a disposal bag, and a travel-size PooPourri Spray. Knowing I had all the supplies I needed to do a quick bag change in a strange bathroom gave me immense peace of mind. I could change the whole system in less than 5 minutes, all by myself!
And if you need a little smile while you fumble around with your first bag change alone, just repeat my favorite mantra out loud: I got this whole thing in the bag!
Lisa Febre is the author of “Round the Twist: Facing the Abdominable,” a memoir about her diagnosis and treatment of Stage-4c Colon Cancer, which hits bookshelves in September 2023. She had a descending colostomy for 10-months.
























































 “golden toilet trophy” engraved like The Stanley Cup! “It was a fun way to get people involved, a good conversation piece for anyone walking by the nursing station,” DuPree says.
“golden toilet trophy” engraved like The Stanley Cup! “It was a fun way to get people involved, a good conversation piece for anyone walking by the nursing station,” DuPree says.














 Exercising with an Ostomy
Exercising with an Ostomy Some people wonder how they can ever find something positive in something so scary as an ostomy, but it can be done. You don’t need to do it in big
Some people wonder how they can ever find something positive in something so scary as an ostomy, but it can be done. You don’t need to do it in big