Sponsored by Coloplast
Have you ever experienced skin issues under your barrier? While peristomal skin conditions are all too common, many are easily treated – and better yet, avoided – with the right knowledge, product fit, and support. Finding the right ostomy barrier to fit your individual needs can be a challenge and may involve trying a few different barriers to fit your unique body and stoma. Getting a nice snug fit between your stoma and ostomy barrier is key to protecting your skin, and helps you reduce the risk of experiencing a frustrating cycle of stoma leakage and resulting skin issues.
If you see an ostomy nurse – great! Every person’s situation is unique, so if you’ve worked together on a solution, or if you’re currently experiencing skin issues that may require a specific intervention, I highly recommend working with your ostomy nurse to find the routine that works for you. That said, below are some general tips that are relevant to anyone with an ostomy.
As the saying goes, “An ounce of prevention is worth a pound of cure” – meaning it’s preferable to take precautions than to suffer the consequences later. This is also true in ostomy care. So, what can taking precautions for peristomal skin health look like? While it may not be realistic to prevent skin issues 100% of the time (after all, things happen!) finding a well-fitted and comfortable pouching system for your stoma and body profile is a great place to start in reducing your chances of skin issues. I always like to explain proper fit like trying on shoes at the store. When buying a new pair of shoes there are different criteria to follow. For example, is this the right size? Is it too big? Too small? Does my foot move around too much or not enough? Does it chafe when I bend too much or too fast? All these questions can also be asked when selecting the fit of your ostomy barrier.
The right barrier?
While you might sacrifice comfort for a number of reasons when you’re picking a new pair of shoes, your ostomy barrier should be treated more like your favorite go-to shoe no matter the occasion – going out on the town, running on the trails, or enjoying a quiet night in. If your shoe doesn’t fit and move with your foot just right, you may find that you have blisters on your heels from walking in them for too long. Similarly, if your barrier doesn’t move with your body while you sit, stretch, and go about your day, you may also find blisters or painful sores underneath your adhesive. That’s why the adhesive of your product is also important to consider when finding the right barrier for you – there are a lot of options out there! For instance, there are options for more stability around your stoma, more flexibility, special sizes and shapes to better fit your body’s contours, more resistance to breakdown from stoma output, and a host of other options that your WOC nurse can help you navigate. No matter which option you choose, an ostomy barrier should move comfortably with your body and shouldn’t limit your activities or range of motion.
Does this fit just right?
A great question! Let’s continue referencing trying on shoes. If the shoe is too large, your foot slides around and can create some friction in some places like your heel or your toes. Ouch! If the shoe is too small for your foot, it’s too tight and is quite uncomfortable, which can also create some friction and maybe some sores, much like when the shoe is too big. So, how do we relate this to an ostomy barrier? Let’s discuss! An ostomy barrier needs to be snug to the stoma and measured properly. If the barrier size is cut too big, the risk of stool or urine on the skin from the fit not being appropriate can create irritation or even sores. If the barrier is too tight, the proper seal may not be achieved, and the improper fit could lead to irritation on the skin or even to the stoma if the fit is far too tight. Just like you would use a previous shoe size as a reference or a foot-measuring size guide at the store, utilizing a stoma measuring guide to size up your stoma may be key to getting the right fitting barrier. You want to make sure that the measuring guide fits snug around the stoma, but not too tight, and just close enough to the stoma so the skin doesn’t show through.
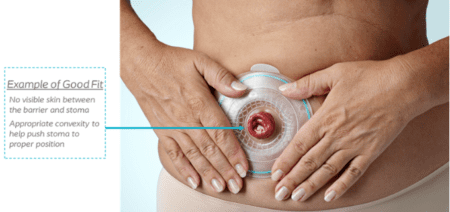
For illustration purposes only. Performance and experience may vary. Talk to your healthcare professional about what may be right for you. Please refer to product ‘Instructions for Use’ for intended use and relevant safety information.
What is a solution?
Finding the right solution may take a few tries to find the right fitting barrier for your body type and your stoma size. When finding the right fit, the goal is to reduce any peristomal skin irritation or issues you could experience from improper sizing. Utilizing a size guide or template that you created is helpful with each pouch change to stay consistent. If the fit of your barrier changes, like after surgery when your stoma swelling goes down, creating a new template may help reduce potential peristomal complications.
Making a routine for fit
Don’t forget to do a body assessment when you perform a stoma assessment. What is a body assessment? Let’s reference shoes again. Just like when you try on a pair of shoes from many years ago that used to be your favorite to wear, you may find that when you try them on, they no longer fit, and it’s time to go up a shoe size. Similarly, it’s important to observe your stoma and skin over time to make sure that the barrier you’re using still fits right. All bodies change over time, especially our skin. Fluctuations in weight and differences in skin texture may impact the fit of your barrier. One way to stay on top of your body assessments is to do an online check. Coloplast’s BodyCheck tool is a simple way to check in on your fit and assess your body and stoma profile. If you feel it has been a while since the last time you checked in with your WOC nurse for a barrier fitting, I’d certainly recommend scheduling an appointment, too. Current guidelines recommend an annual checkup with a WOC nurse, and this is a great way to get back on track with your fit.
 Mackenzie Bauhs, CWOCN, is currently an employee and Ostomy Clinical Consultant for Coloplast. She obtained her bachelor’s degree at Carroll University in Wisconsin. She has worked with ostomy patients in the post-operative period at the University of Wisconsin Hospital and Clinics in Madison, Wisconsin as well as outpatient ostomy care at Rush University Medical Center in Chicago, Illinois.
Mackenzie Bauhs, CWOCN, is currently an employee and Ostomy Clinical Consultant for Coloplast. She obtained her bachelor’s degree at Carroll University in Wisconsin. She has worked with ostomy patients in the post-operative period at the University of Wisconsin Hospital and Clinics in Madison, Wisconsin as well as outpatient ostomy care at Rush University Medical Center in Chicago, Illinois.
The materials and resources presented are intended to be an educational resource and presented for general information purposes only. They are not intended to constitute medical or business advice or in any way replace the independent medical judgment of a trained and licensed physician with respect to any patient needs or circumstances. The information presented or discussed may not be representative of all patient outcomes. Each person’s situation is unique, and risks, outcomes, experience, and results may vary. Please see complete product instructions for use, including all product indications, contraindications, precautions, warnings, and adverse events.
Editor’s note: This article is from one of our digital sponsors, Coloplast. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.