My Ostomy Story
Hello! My name is Marcia Benedict. I have a urostomy due to bladder cancer.
Facing an ostomy and what life would be after surgery can be overwhelming and I found myself repeating, “I never expected this”. I was dumbfounded, speechless; and at first, all I could do was cry. I hope my story will give you the strength, support, and desire to thrive beyond expectations.
My Journey
After retiring to Tucson, AZ in 2019, I remembered hearing, “if you ever find yourself in need of medical attention and don’t know who or where to turn, search for the nearest teaching hospital”. I sought medical attention at Banner University Medical Center. The support from doctors and their care team, my Ostomy nurse (CWOCN) and our local Ostomy Support Group has been invaluable.
Despite the initial fear and challenges, I adapted to my new normal by being my own best advocate. I needed to speak up, be determined and resilient.Through it all: Urogram, cystoscopy, cytology, TURBT (transurethral resection of bladder tumor). Diagnosis: T2/T3 tumor of the bladder invading the vaginal wall. Treatment: chemotherapy, radical cystectomy and hysterectomy. Recovery: one day at a time. Time for emotional and physical healing, following doctors’ orders, being kind and patient with myself. I survived each step, repeating each as needed along the way, and so can you!
Be Prepared – a Few Hints and Hacks
As I was living alone and my cat was not proficient in nursing duties, I requested skilled nursing rehab (SKF) upon hospital discharge. Though my surgeon recommended recovery with home health, he understood my dilemma and helped make those arrangements through his nurse navigator and case manager, followed by home health services (visiting nurse, PT/OT, nutritionist) when I returned home.
Support was such a lifeline in helping me better understand and cope,
Before surgery, I ensured I had a waterproof mattress pad, chux (puppy pads) for my bed and bathroom. Upon discharge from SKF and home health therapy, I preordered my ostomy supplies with the help of my WOC nurse. Over time, I became efficient in changing my pouching system, reducing the time from over an hour to now 15 minutes. Practice makes perfect (most of the time). Despite initial challenges, I adapted with determination. I set alarms on my phone to remind me to empty my pouch and avert potential leaks. Just in case, I always carry a puppy pad under the front seat of my car. To this day, I have repeat calendar schedules to change my pouch. Once, driving on the Interstate, I improvised with an empty water bottle as a makeshift urinal when restrooms were closed during the pandemic. I also keep an empty disposable water bottle (with the cap) in my car and a complete pouch change packet in my purse or backpack. These experiences taught me valuable lessons and have helped me manage with confidence.
You Are Not Alone
Two days before my surgery at the suggestion of my WOC nurse, I went to an Ostomy Support Group, a local affiliate of UOAA. To my surprise, I walked into a roomfull of ostomates of all types. They were welcoming. In a roundtable setting, they talked about the facts, the foibles and the freedom of living with an ostomy. They gave me strength to face what was coming and faith that there was life after ostomy surgery.
That first meeting led me to fulfill one of my retirement goals: …to give back by helping others facing similar journeys. Recovering during the pandemic, in-person meetings were cancelled. Support was such a lifeline in helping me better understand and cope, I signed up as a phone contact. The Local Group initiated monthly Zoom meetings; and when restrictions were lifted, in-person monthly meetings reconvened.
I’m excited to be attending for the first time this year’s UOAA National Conference in Orlando. I’ve heard from previous attendees the information is educational, inspiring and a good time is had by all. I look forward to meeting some of the wonderful UOAA personnel who have helped me along my journey. Enough can’t be said about their resources: tips, educational publications, particularly the “Living with a Urostomy” guide online, supportive Ostomy Academy discussions and video sessions. If you haven’t tapped into the website www.ostomy.org or the UOAA Facebook page, I encourage you to check it out.
The Future

Initially, everything was daunting, but my expectations for retirement and recovery have exceeded my dreams. I’m healthy, happy and fearless.
Despite the initial fear and challenges, I adapted to my new normal by being my own best advocate.
Surrounded by family and friends, I’m active. I play golf, swim, and dance again. I travel by car, plane, and train in the U.S and internationally. Supplies and all, I braved a 26-day cruise. I even rode a camel!
Wherever I go, my “Bathroom Access Card” is in my wallet, and translated in 2 foreign languages on my phone. In recovery, I found the time and strength to redesign and renovate my kitchen. Made time to socialize. I recently attended my oldest granddaughter’s college graduation and all the festivities. I’m looking forward to it all over again with my second granddaughter who is studying medicine. Since my surgery, I feel blessed indeed, going on 6 years NED (no evidence of disease).
And I’m no longer single! I have a wonderful relationship with a man who adores me for who I am, including my ostomy. There is little to keep me from a fulfilling life, and you shouldn’t let a pouch stop you either.
You’ve Got This!

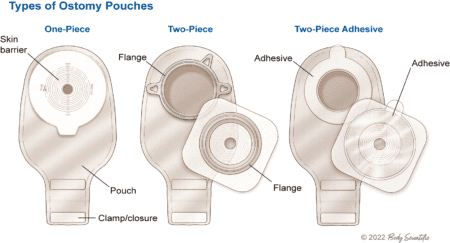 The ostomy nurse had a lot of information to cover in a short period, and she thought all of it was important. Afraid of failing, I was certain that I was going to make terrible mistakes. I doubted my ability to do any of this.
The ostomy nurse had a lot of information to cover in a short period, and she thought all of it was important. Afraid of failing, I was certain that I was going to make terrible mistakes. I doubted my ability to do any of this.