A Second Opinion Leads to a Life-Changing Ostomy
 In the spring of 2014, I had completed another colonoscopy for my ulcerative colitis. It was my fifteenth colonoscopy in twelve years and many prescriptions of drugs later to curtail the bleeding of the polyps in my intestine.
In the spring of 2014, I had completed another colonoscopy for my ulcerative colitis. It was my fifteenth colonoscopy in twelve years and many prescriptions of drugs later to curtail the bleeding of the polyps in my intestine.
I had a very productive career and life with a CPA practice for 34 years. In Grapevine, Texas I served on the school board and as a city council member, and was named “Citizen of the Year.” But bleeding and bathrooms were getting on my nerves, so I called the Mayo Clinic in Rochester, Minnesota, unbeknownst to my gastro doctor. I told them that I wanted another opinion.
After four days of extensive tests, discussions, colonoscopy, the doctors at Mayo concluded that the polyps were entirely too large to remove by minor surgery without bigger risks, and that removal of my large intestine was recommended. Cancer was discussed at length including risks and possibilities with large polyps and various medical unknowns involving my circumstances.
My large intestine was removed January 4, 2015. The surgery was in my home town and I had a great ostomy nurse that taught me all of the intricacies of the ostomy pouch and supplies. I returned to retirement life again here in the Mountains of Texas where it is cool in the summer and we return to Grapevine for the winter where we had our careers.
I am 76 today and walk with my dog 3 to 10 miles each day. I play golf anytime I can. I am very active in my small town and I play the organ at our church each Sunday. I am not overweight and enjoy eating most anything. I find it necessary to chew every piece of food very well. I avoid nuts, corn, kale, popcorn, and tough fruit skins.
I love life and I am so happy for the decisions I made.
Saturday, October 3rd, 2020 marks the 10th anniversary of Ostomy Awareness Day. In partnership with United Ostomy Associations of America (UOAA), Hollister Incorporated is proud to stand with the entire ostomy community in celebration. Every ostomate has a voice worth hearing and we aim to embody ostomy confidence of our worldwide community with #OstomateVoices.
Spread Positivity and Share Your Voice

We’re connecting and empowering our worldwide ostomy community to share their own unique experiences—their challenges, their achievements and the joys of their daily lives. Share your words of encouragement that have helped you along your ostomy journey. Your story might help someone who might be struggling. Using your words, we’ll create a unique social card that you can share with your friends, family, and community. Share your voice here!
Join Us for a Virtual Cooking Class

Join us for a virtual cooking class on October 3rd with private chefs Ryan Van Voorhis, a fellow ostomate, and Seth Bradley of Nude Dude Food™, one of Chicago’s most sought after private dining and catering services. Register today to connect with others in the community and cook a delicious meal. Register today!
For more resources on nutrition with an ostomy, check out UOAA’s Food Chart or download the “Eating with an Ostomy” Nutrition Guide.
Show Off Your Stoma Sticker

Stoma stickers are a great way to raise awareness, start a conversation, or show support. Order your free Stoma Stickers in time for Ostomy Awareness Day, shipped anywhere in the US.
Share a photo or video of your Stoma Sticker on social media using #StomaSticker to be part of the conversation. Or show off your Stoma sticker while running in your virtual Run for Resilience Ostomy 5K and share how you celebrated #OstomyDay2020.
Share your #OstomateVoices and personalize your next Instagram or Facebook Stories with the Hollister “Ostomate Voices” digital stickers. It’s easy – search “Ostomate Voices” in the GIF library when creating a Story and you’ll find the whole collection, including a UOAA lifesaver and Stoma Sticker!
For more resources and interactive ways to get involved, visit Hollister.com/ostomyawareness.
Editor’s Note: this blog post was provided by Hollister Inc. the exclusive Diamond Sponsor of UOAA’s annual Run for Resilience Ostomy 5K events that benefit UOAA, a 501(c)(3) nonprofit organization.
A Decade of Shining a Positive Light on Lifesaving Ostomy Surgery
By Jeanine Gleba, UOAA Advocacy Manager
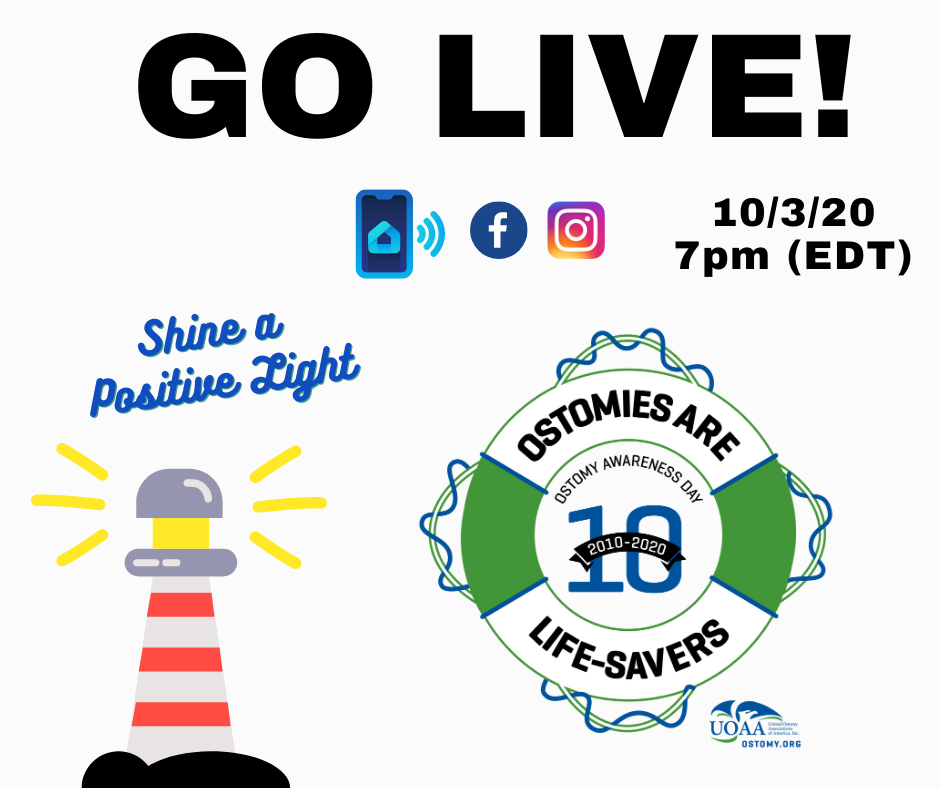
“Ostomates Unite and Help Place The Ostomy In A Positive Light! Celebrate UOAA’s Ostomy Awareness Day!” These were the words that were spread when UOAA announced the first National Ostomy Awareness Day on July 25, 2010. A decade later, UOAA continues to sponsor and celebrate this day annually in the United States by raising awareness about this life-saving surgery and increasing national visibility of those living with ostomies. Starting in 2014, and all subsequent years, UOAA has been celebrating Ostomy Awareness Day on the first Saturday of October, which coincides with World Ostomy Day every three years. This year National Ostomy Awareness Day will be held on Saturday, October 3, 2020.
The idea for an awareness day was originally suggested by Ally Bain, who worked with UOAA as a summer intern in 2010. (Flash forward, this is the same Ally instrumental for the Restroom Access Act (aka Ally’s Law). The awareness day began as an experiment in social media to see what kind of grassroots support they could get for ostomy recognition. UOAA sent out a request on social media asking all followers to show their allegiance to the cause by changing their online status to the slogan above and make their profile picture UOAAs logo. The immediate response was so strong that they were also contacted by friends at Talkin’ Bout Guts, to host a 24-hour live podcast in honor of ostomy awareness. Thousands participated that year.
In recent years, UOAA has also named an Ostomy Awareness Day Champion. This year’s champion is Robin Brown, pageant winner Mrs. Washington, who uses her stage platform to raise awareness for ostomy surgery “all in the hopes that it can be a light for someone stumbling in the darkness”. Her ostomy story and journey from farm girl to the title of Mrs. Washington World America is inspiring. Watch her special video message for Ostomy Awareness Day!
Over the years, celebrations have been centered around several different themes including Bouncing Back into Life, Navigate the Journey Together, Speaking Out Changes Lives and, most recently, Ostomies Are Life-Savers.
To commemorate the 10th anniversary, here are 10 ways you can join the movement to raise ostomy awareness this year:
- Help shine a positive light on ostomy surgery and go “live” on your own at 7:00PM EDT on October 3rd with people all across the United States. Hit the “live” button on your personal social media accounts (Facebook, Instagram or TikTok) to shine a light on yourself and tell everyone how your ostomy saved your life or that of a loved one. If you are a medical professional, share how your work helps save lives.
- Participate in our 7th annual Run for Resilience Ostomy 5k. This year our local Ostomy 5k events will be held virtually along with our annual worldwide virtual Run/Walk, so you can walk or run in your favorite place or at home. Visit www.ostomy5k.org to register or donate for one of these events. You can also join UOAA’s “United Advocates Smashing Stigma” team too!
- Create a fundraising team through one of our Ostomy 5k events and challenge your family, friends, Affiliated Support Group members, colleagues and coworkers to raise ostomy awareness and funds for a good cause! Have your teammates share the team campaign and see who can get the most donations. Better yet, ask your employer to match any donations raised!
- Make a donation to the “Ostomy Awareness Fund” as a tribute to the 10th anniversary. Donate a minimum of $30 and receive a special bandana with the “Ostomies Are Life-Savers” graphic image. These bandanas are also a great pet accessory. Share a photo with UOAA of your pet raising ostomy awareness!

- Participate in some of the events we have planned with partners such as the Facebook Live Event that will be co-hosted with Crohn’s and Colitis Foundation on October 3rd.
- Raise awareness and spread the message that ostomies are life-savers using our infographic. We encourage you to share, post or print it wherever possible.
- Our Operation Ostomy – A Life Saver campaign continues to spread the message that we are saving lives one ostomy at a time. Please use our 10th Anniversary Ostomy Awareness Day logo for your profile picture on your social media accounts. Use the hashtags: #OstomiesAreLifesavers #OstomyDay2020 and tag UOAA on Facebook @uoaainc Instagram @uoaa_ or Twitter @uoaa.
- Get your Federal, State or Local elected officials to pass a proclamation declaring October 3, 2020 as the 10th anniversary of this special day. Use our sample proclamation or take action here.
- Use our sample letter to the editor to share with your local media why ostomies are life-savers.
- Aside from Ostomy Awareness Day, October is full of fun fall activities. Carve a pumpkin (or paint) in an ostomy theme. “Shine a light” in your carved pumpkin and raise ostomy awareness in your neighborhood.
For more information and the latest ways to get involved including activities from some of our sponsors visit https://www.ostomy.org/ostomy-awareness-day/.
With your help we will carry on breaking the silence and shining a positive light on what has saved so many lives.
Living with an Ostomy and IBD led her to become an Unexpected Beauty Queen and Advocate
Hi Everyone! My name is Robin Brown, I’m a 40-year-old wife, momma & farm girl. I also happen to have an ostomy and the title of Mrs. Washington World America!
My relationship with my guts has been a long battle….even as a child I suffered from severe ulcerative colitis symptoms but I wasn’t officially diagnosed until I had my first bowel resection at age 21 as result from an infection following an appendectomy. I lost my marriage and some guts but I finally got some answers…or so I thought. The next ten years were a rollercoaster of medications, treatments, alternative therapy and surgeries(15 to be exact.)
 I was miserable. My family was miserable. But, I’d had enough and didn’t want any more treatments. Soon I was back in the hospital and one doctor reviewed ALL my info and said he knew exactly how to fix me…OK, just one more surgery then. Well, he was right…he fixed me!! I was no longer having incontinence issues, I could eat again (personalized diet plan) and was feeling great compared to the previous ten years. End of story right?!
I was miserable. My family was miserable. But, I’d had enough and didn’t want any more treatments. Soon I was back in the hospital and one doctor reviewed ALL my info and said he knew exactly how to fix me…OK, just one more surgery then. Well, he was right…he fixed me!! I was no longer having incontinence issues, I could eat again (personalized diet plan) and was feeling great compared to the previous ten years. End of story right?!
WRONG! Less than a year after surgery I was in an accident where I was crushed between our off-road truck and the back wall of our garage. It was a literal and figurative blow that nearly took my life. I had holes in my large intestine, holes in my small intestine, a shattered pelvis, four broken bones in my back and an aortic aneurysm. I had to undergo countless operations, hours of physical therapy and I was even put into a coma while doctors worked fixing one piece at a time.
After everything began to heal I realized how broken I was. After the accident, I lost myself. I had worked as a medical assistant for years and loved working in healthcare. Now that was gone. I was finally a mother after trying for nearly ten years. Now I couldn’t even lift my two-year-old son for a hug. I took great pride in being a partner to my husband. Now I needed him to help me sit on the toilet. I was stressed and depressed. My UC symptoms worsened by the day and now that I had shortened guts it caused a multitude of other problems like rectal prolapse (twice!) which led me to finally agree to get my colostomy pouch. I cried, a lot.
Being home, then in and out of the hospital, and no longer able to have a 9-5 job I decided to start a little online business selling skincare and cosmetics. Not really to make money but just to feel like I was doing SOMETHING! I had to get out of this funk. I was hiding. Hiding from my husband, even though he had an easier time accepting things than I did. Hiding from my reflection- because every time I saw myself I felt depressed and sad. I was hiding from the world by wearing bulky sweatshirts in the middle of summer so no one would see my bag. Then one day in my online makeup group I shared a bit of my story. The response was amazing and beautiful and that’s when things began to shift. One afternoon I received a message from an old friend suggesting I compete in a Mrs. Beauty pageant since the focus is so much on what you do to inspire rather than just what you look like. Me? In a pageant? Probably not. Then a few weeks later the same suggestion from another. Ok universe…I hear you. I decided to apply for the Mrs. Washington America pageant and was quickly named Mrs. Mason County.
Great! What in the heck did I sign up for? Before surgery, I swore off swimsuits and anything tightly fitted. Now, not only will I wear a swimsuit on stage but I’m going to ask to be JUDGED?!?! What on earth was I thinking? Now, in addition to volunteering and fundraising, each queen must have a platform. Something they want to bring awareness to and are passionate about. The obvious choice for me was gastrointestinal disease and ostomy awareness and education, but that’s not the most beautiful platform and can make people uncomfortable. As quickly as the idea came, fear and doubt began to creep in and I promptly began thinking of other ideas.
At my first pageant event, a holiday party to meet all the other queens, we were introduced to a designer that would be custom designing an opening number dress for each of us! As I chatted with the designer I quietly mentioned I had a colostomy bag and could we design something to hide it as much as possible because I wanted to feel beautiful. A short while later I bumped into a sister queen at the elevators. She introduced herself and wanted to know if she could ask a personal question…of course, I said! She asked if she overheard my conversation correctly that I had a colostomy bag? Yes, yes I do! “Really?!? Where, I don’t see it?” She continued, “are you happy you made that choice? What’s the hardest part? Does it hurt?” A million questions rolled off her tongue at once and then she shared her struggles with GI disease and the fact that an ostomy has come up in her doctor’s appointments and she was terrified and thought life would be over¬– until she met me! I knew right then, I had the right platform and that by sharing my story I could help others in ways I never dreamed.
At that moment a woman approached. She wanted to let me know her husband has an ostomy and seeing me on stage gave them so much hope and even though I didn’t win they were cheering for me! Again, I had to thank the universe for letting me know I was exactly where I was supposed to be.
In the months leading up to the pageant, I began volunteering at hospitals and schools, sharing about differences and acceptance. I had the opportunity to be a speaker with a major medical company to share my ostomy journey and provide input to how they can better serve our community. I even went live on Facebook and showed my bag to the world!
In a few short months, I became empowered and proud of my body and my spirit again. I walked the stage in a swimsuit like I was a supermodel, rocked a gorgeous FITTED gown with grace, and with a smile heard myself say the word bowels, as it proudly rang through the pageant auditorium.
 Guess what? I didn’t win. I did not even place in the top 10. I went to the coronation party with a stage smile and promptly excused myself with my best friend by my side. She knew I needed to cry. As we reached the bottom of the grand staircase I could feel the tears of disappointment welling, and her hand grasping tighter to my arm letting me know I just had to keep it together for a few more seconds. At that moment a woman approached. She wanted to let me know her husband has an ostomy and seeing me on stage gave them so much hope and even though I didn’t win they were cheering for me! Again, I had to thank the universe for letting me know I was exactly where I was supposed to be.
Guess what? I didn’t win. I did not even place in the top 10. I went to the coronation party with a stage smile and promptly excused myself with my best friend by my side. She knew I needed to cry. As we reached the bottom of the grand staircase I could feel the tears of disappointment welling, and her hand grasping tighter to my arm letting me know I just had to keep it together for a few more seconds. At that moment a woman approached. She wanted to let me know her husband has an ostomy and seeing me on stage gave them so much hope and even though I didn’t win they were cheering for me! Again, I had to thank the universe for letting me know I was exactly where I was supposed to be.
Soon after, I applied to represent Washington at the Ms. World International pageant after a few weeks and committee meetings later, I was selected! I am now Mrs. Washington World America and I couldn’t be more proud to represent my state and the ostomy community at the upcoming pageant.
I never thought I’d have an ostomy. I never dreamed this farm girl would be a beauty queen. I never imagined my trials would become my triumph and my story of hope. Throughout my life, many have attempted comfort me with the words “everything happens for a reason.” This honestly just kept me waiting for a moment of clarity and answers but that moment never came. I found no reason! I think sometimes bad things just happen and it’s up to us to give them meaning and purpose. For me this is it. Sharing my story, my triumphs, my tragedies. All in the hope that it can be a light for someone stumbling in the darkness.
Robin Brown will be this year’s Ostomy Awareness Day Champion for UOAA. Check out all the ways to get involved and join with her on Saturday, October 3, 2020.
Bladder cancer and urostomy surgery do not stop Annemarie from living her best life.
I am a bag lady. I am highly educated and employed, yet carry a bag wherever I go. I don’t leave home without it. Because of bladder cancer, I have a urostomy. Like many other women, it took some time for my diagnosis. At 57, many of the symptoms I experienced were attributed to my age: menopause, UTIs, kidney stones, fibroids, etc. Thanks to the fibroids, I was scheduled for an ultrasound. It was my gynecologist who found the bladder tumor. She referred me to a urologist. In fact, she insisted. Her office called to make sure I followed through. I met that week with a local urologist. He did a scope. I saw him look at the nurse, concern written on both their faces. He started talking about surgery and apologizing for the diagnosis. In my naivete’, I had gone to the appointment by myself. I don’t remember him even saying the words, but I had bladder cancer.
Scans and a transurethral resection of a bladder tumor (TURBT) were scheduled for the following week. Usually an outpatient procedure, I was in the hospital for 4 days due to heavy bleeding after the TURBT. The tumor was large and the doctor couldn’t get it all but he thought it had penetrated the muscle. Unfortunately, the pathology was inconclusive so he did another TURBT the following week. The outcomes were exactly the same so we both decided my best chances were for a second opinion at Dana-Farber Cancer Institute in Boston. Throughout our discussions, he explained what my future might entail. It looked likely that they were going to have to remove the bladder and I would either have a new “bladder” or a bag. Quite honestly, I had no idea what it entailed, but I was horrified.
Dana-Farber is an amazing place. I had a whole team in place: a medical oncologist, an oncology urologist, a nephrologist, among others. The plan was an MRI to confirm the tumor’s pathology, a nephrostomy tube, chemotherapy and, if the cancer had not spread, a radical cystectomy. If it had spread, I would not need surgery but would be eligible for palliative care. Who would have thought surgery is the best case scenario. Due to claustrophobia, and despite anesthesia and Ativan, I moved so the MRI was inconclusive. I needed another TURBT. Thanks to my new amazing surgeon, the tumor was removed and the passage to my kidney was cleared. The pathology of the tumor showed no spread to the muscle and an ultrasound showed no more kidney hydronephrosis. Even better, I would no longer require chemotherapy. I did try immunotherapy with BCG but it did not work. The cancer was aggressive so we had to treat it aggressively. My radical cystectomy was scheduled for January 25, 2019.
It took me a long time to get there. I even asked what would happen if I did not receive the surgery. I would be dead in a year.
Wow, that was sobering. Because of the proximity of the tumor, I did not qualify for a neobladder. I would have to have a urostomy. Every time I talked about it, or even thought about it, I cried. I felt like I was going to be a freak. I offered my husband a divorce if he wanted one. I was devastated and frightened. I have learned that fear of the unknown and our imaginations are far worse than the reality. While so much of what had happened to me was out of my control, I did have control over one thing: HOW I handled everything. I decided knowledge was power. I was fortunate. My hospital had a class for urostomy candidates. For the first time, I was able to see an actual urostomy pouch. I was given hands-on instruction on how to change a bag. I met ostomy nurses (the best people in the world!) who would be helping me.
I decided I would be the one to handle my changes, right from the start. I would take control.
My surgery lasted 7 hours. I needed a transfusion but things went well otherwise. The surgery was not easy. People have described it as feeling like you were hit by a bus. I never really had any pain. It was easily managed with Tylenol. However, I was so weak. I eventually needed an iron transfusion. The one thing I wish I had gotten for my return home was a shower chair. Showers were the worst for me. It took me two months to feel more like myself and another month before I felt ready to return to work. I also cannot say enough about getting a good ostomy nurse. I have been described as a delicate flower (surprising to those who know me). I have very sensitive skin. The nurse was a Godsend to me in trying to manage all of my skin issues. After my visiting nurse visits ended, I continued to see the ostomy nurses at the hospital where I had my surgery. It took a year but, through trial and error, I finally have gotten a handle on things.
I had a few leaks. They were usually caused by user error. They were not the huge floods I expected. Honestly, none of this was as awful as I expected. So many people said this would be my “new normal”. I can’t stand that term. I call it my new reality. There isn’t anything normal about having a urostomy. However, it is very doable. I now wear two-piece bathing suits. I didn’t before. I am wearing the same clothes as I did before. I can kayak, hike, ride my bike, swim for hours, anything I did before. I was here for the birth of my first grandchild. I am back to work, a job that I love. I am not shy about talking about my bag to others. It is not a secret. In fact, I am kind of proud of it. I am alive and life is good.
 Finding Hope in the Stories of Others
Finding Hope in the Stories of Others
By Scott Steehn
All stories have a beginning, and mine is no different. It started on a cold, slate-colored February day in Erie, Pennsylvania in 1992. I was a successful standup comic who had headlined clubs and theaters in all 50 states and seven foreign countries. I was recently engaged to my soulmate, and we were making plans for a big October wedding. I was just finishing up a great week at a terrific comedy club in Erie and, as I prepared for my two shows on Saturday night, I felt like everything couldn’t have been going any better. But, in just 12 hours, none of those things would matter.
It started when I was onstage during the first show. I began having abdominal pain on my left, lower side. It wasn’t a huge pain and mainly felt like a had a fairly intense need to move my bowels. I finished up my show and made a beeline to the restroom. And…nothing happened. Nothing at all. The NEED was still there, and, in fact, it was getting worse. I, of course, had been constipated before, but this felt somehow…different.
I did my second show, but the pain was now almost unbearable. I headed back to my hotel, stopping only at a drugstore to pick up a laxative. I had convinced myself it was just constipation and had even assigned the blame to the shrimp dinner I’d had the night before. “Fresh Shrimp” in February…in Erie?! What did I expect to happen?
I took the laxative. And I waited. And tried. And waited some more. And then the pain got bad. Real bad. I could barely walk and couldn’t move without intense pain shooting out from my left side. Now I had a new theory. Burst appendix. This was before the days of Web MD, and I was limited to only what my imagination could conjure to freak myself out. So, not wanting to die a ridiculous death in the Erie Hilton, I called a taxi and headed to the hospital.
They got me into an exam room in short order. The doctor examined me and, taking advantage of his fancy medical degree, immediately eliminated appendicitis. So much for that. He then told me he had an idea what it was but wanted an MRI to confirm the results. A quick trip through the “donut of doom” confirmed his initial diagnosis. It was something called diverticulitis. He explained how we all have small abscesses in the colon and how they usually don’t cause any problems. Sometimes, however, those abscesses become infected. It causes horrible pain and constipation, and once it gets this bad, it has to be treated with antibiotics and mass quantities of fluids. I spent a painful week in the hospital and was discharged with very specific instructions on how to adjust my diet and lifestyle to prevent a recurrence. I thanked all the staff for the great job they did, signed some papers, checked out…and promptly ignored his instructions for the next 20 years.
Christmas Eve, 2012. My wife has had enough. The final straw came when I was unable to make it upstairs for the family gift exchange. As soon as it was over, she came down and told me we were going to head to the emergency room. I didn’t have the energy to argue. Plus, I knew she was right. I’d been feeling terrible for almost three years. Something was definitely not right. It seemed like it emanated from the “diverticulitis spot” that I had become intimately familiar with due to the flare-ups I suffered through two or three times a year. The only confusing part was I had undergone a colonoscopy six months prior and had received a clean bill of health. Only much later did I learn that I had received a negligent result. My doctors all agreed- there was no way my problem could have been missed.
I should have known I was in trouble when, after the emergency room doc saw me initially, he asked me if I’d like anything for pain. I jokingly said, “Sure, how about some morphine?” He immediately replied, “Okay, we’ll get that going for you.” Uh oh. A little later he told me I had a blockage that had been caused by a buildup of scar tissue from the repeated flare-ups of diverticulitis. They needed to get rid of the infection and then remove the two damaged sections of bowel. Surgery was scheduled for New Year’s Eve. Merry Christmas and Happy freaking New Year!
I spent the next week in a morphine haze. I met my surgeon, a brilliant young lady who looked impossibly young for someone with that much schooling. She explained that they were hoping to remove the damaged sections laparoscopically. It was a relatively simple procedure that would require a couple of days of recovery in the hospital, a week or two at home, and then back to my normal life. The alternative would be invasive surgery, much longer recovery time, and, while the healing took place, I would need to have a colostomy. Due in part to my opiate fog and also due to my refusal to accept reality, I was 100% convinced everything would be done laparoscopically. No worries.
The first thing I noticed when I came to was something in my throat. Something huge and foreign. As my world blinked into focus, the nurse was there to explain to me that the damage was much worse than they had anticipated. Full surgery had been performed and I was going to be in the hospital for a while. The drugs were very helpful in allowing me to deny exactly what exactly that meant. I was much more concerned with getting the tube out of my throat and the catheter out of the other end. That cavalier attitude about my situation would soon change.
The nurses and staff were great. They changed my colostomy bag for me and allowed me to STILL not grasp my situation. That all changed when I met the ostomy nurse. She was tasked with teaching me the intricacies of daily life with a colostomy. Reality came crashing through the door when I spent 30 minutes hiding in the restroom in tears unable to change my bag. I can’t do this! This isn’t fair! (Conveniently forgetting the 20 years I had spent ignoring my doctor’s orders) Gathering myself, I sucked it up, and FINALLY was able to do it on my own. I was discharged and sent home to recuperate and heal for 30 days before heading back to the hospital for takedown surgery.
I’d like to tell you a story about how well I adjusted. About how I was brave. About how I was thankful to be alive. About how I now appreciated my friends and family even more. About how I would now refused to take all the beauty of life for granted. That’s the story I’d like to tell. But I can’t. It would be a lie. Even though none of you know me, I promised myself I would be 100% honest about my journey. Warts and all. So here goes.
It was awful. I hated every minute of it. I thought having a colostomy was gross. And hard. Life wasn’t fair. NOTHING was fair. I can’t do this. There were the usual indignities. Accidents. Broken seals. Excess gas. I was in hell. Never for one moment did I think how my situation affected those around me. How my actions and attitude affected my family, and, my wife in particular, who only wanted me to get better and get back to being the man she married. As an added bonus, I was also taking 12 Oxycodone a day for pain, and, rightly suspected, now had a raging opioid addiction. My day consisted of sleeping, crying, bitching at my family, thinking about death, and dealing with my new, hated, appendage. Day after day. Rinse, lather, repeat.
Then, one day while noodling around on the internet, I found UOAA. I started reading about my condition. And I started reading other people’s stories. I found out just how many dealt with this particular challenge. I was stunned. And the more stories I read, the more my respect grew. People who had to deal with this for years. For decades. Tears streamed down my face as I read their stories. I’d love to tell you everything changed that day. How my attitude changed overnight and how I became Mr. Positivity. Alas, it wasn’t that simple.
What DID happen, is I became embarrassed about my actions. I had always prided myself on being a tough guy who dealt with problems head-on. The more I read on ostomy.org, the more I knew this was a lie.
Every day I read the stories of real heroes. Men and women who possessed the biggest superpower of all, the ability to live a normal life despite adversity that was currently bringing me to my knees. To say they inspired me, would be an understatement. Closer to the truth would be, they saved my life.
They gave me practical advice, “insider tips” on everything from bathing to sex, and something I hadn’t felt in a long time. They gave me hope. I never posted on the UOAA discussion board. Hell, I don’t think I even registered. Due to my “temporary” status, I really didn’t think anyone wanted to hear my whining. If everything went well, my life would go back to “normal,” while these people would continue to lead quietly heroic lives day after day, year after year. I didn’t feel worthy. And I still don’t.
That’s my story. Sure, there’s more, including an unsuccessful takedown, massive infection, emergency surgery, and an ileostomy for a few more months. There was a wound vac, and an in-home nurse to change my dressing daily. And, of course, after 6 ½ months of daily opioid use, I still had to deal with that King Kong-sized habit. Yet, in the end, I was okay. It probably took almost two years to feel like me again. And even that isn’t completely accurate.
I recovered, I felt better physically, but “myself” was different. I was more appreciative, more humble, and more thankful. I was well, but I’d never be the same.
So, thanks for reading. Thanks to Ed Pfueller for giving me an opportunity to share my story. Thanks to the whole team at UOAA and, for that matter, all of the sites designed to educate, inform, and help everyone on this particular journey. Lastly, more thanks than I could ever express to all the men and women who bravely shared their stories through blogs and forums. Thanks for your bravery. Thanks for your humor. And thanks for giving me the courage to understand and accept my condition with, what I hope, was grace and determination that would make you all proud. God bless each and every one of you and may your lives be full of the joy and love that you so richly deserve. I am forever in your debt.
Imagine being your 15-year-old self again. What did that feel like? Young, carefree, happy…healthy?
For me, I felt all of those things every day. I played the clarinet, got good grades, was athletic from running track, active in school/church clubs and had amazing family/friends. What more could I want as a teenager?
I didn’t want for anything until one day I no longer felt like my healthy self anymore and all I wanted was to be healthy again. This is when my life changed forever…
It was November of 2012, at the time I had just moved to Los Angeles, California with my mother from Maryland. I was very excited to move and support my mom with her new job opportunity. She is like my best friend and nurturer at the same time. It was always just her and I growing up, no siblings. California’s scenery was colorful and vibrant. All I could picture were the great things my future would bring living there.
That picture flipped upside down within weeks. I could feel my stomach expressing to me that it didn’t like the chicken nuggets or the pepperoni pizza, I was feeding it. Sharp pains that felt like knives were sticking me each time I would eat, pushed me to never want to pick up another piece of food again. No over-the-counter medicine could relieve the amount of pain I would feel. Sick little me sat helplessly with my mother by my side in Ronald Regan UCLA Medical Center’s emergency room waiting to be admitted and seen by a doctor. I thought to myself, “What was happening to me? I don’t understand.”
I couldn’t understand. I was just fine a month ago. My mom was just as confused as I was. The doctors weren’t transparent enough with my diagnosis and had trouble figuring out what was the actual problem. After a few tests, I was diagnosed with ulcerative colitis/Crohn’s disease. This diagnosis soon changed once the gastrointestinal team at UCLA Medical Center (UCLAMC) realized it was strictly my colon that was being affected which changed my diagnosis to ulcerative colitis.
I had no idea what ulcerative colitis was nor had I ever heard of it before. My current gastroenterologist, Dr. Ziring, asked who in my family had the disease but I wasn’t familiar with anyone. My father, mother, and grandparents didn’t have any trace of ulcerative colitis. It was concluded that the change in climate and stress could have taken a toll on my body to make me flare-up. I couldn’t eat certain foods anymore. I was prescribed all types of medication that I had never seen and forced to take pills that were pretty huge to swallow.

Lacee Harper with her mother.
Nearly one month spent in the hospital, my routine had changed. I would wake up take my meds first, eat (liquid-solid foods), watch TV, read a book, walk around to gain my strength and repeat at least three times a day. Once I was released, I remember being so happy to be a normal person again. That feeling went away when my mom took me to buy nutritional drinks to restore my protein, vitamins, and minerals. I couldn’t fit into any of my clothes from the amount of weight I lost and my toned body went away. Dr. Ziring told me that I would live with this forever because there is no cure, which I didn’t want to believe. All I could do was try to understand and educate why my body reacted the way it did to certain foods, activities and mental stability.
Fast forward to 2013 where I moved back to Maryland with my mother, I was enrolled back in my previous high school and actively seeing, pediatric gastroenterologist, Dr. Oliva-Hemker at John Hopkin’s hospital. I couldn’t do any of the previous extracurricular activities I participated in and could only workout at a minimal intensity due to my low blood counts. Throughout the school year, I experienced many flare-ups and trial/error with different medications. Some hospitalizations were longer than others and overtime I became stricter with my diet to prevent excessive flare-ups. My high school graduation wasn’t the best time for me because I was experiencing a severe flare-up that interfered with my ability to keep food down. I missed my senior week summer trip to recover in the hospital and get back to feeling better again.
After graduating from high school, I switched gastroenterologists since I was considered an adult. Dr. Rosen had been my mom’s gastroenterologist for years so the transition was smooth. I was stabilized on Humira and Prednisone throughout my community college career. By then, my mother and I had moved to Atlanta where the weather was nicer. I think the weather, being around family/friends and less stress I experienced helped my flare-ups calm down living in Atlanta. I truly enjoyed my time there and experiencing college at Georgia State University, as well as working part-time.

Lacee recently graduated with a master’s degree from the S.I. Newhouse School of Communications at Syracuse University.
Once I completed my first two years of college and received my associate’s degree, I transferred to Syracuse University (SU) to achieve my bachelor’s degree. This was one of the hardest transitions of my life moving from the South to the cold North. My third year of college and first-year being away at a university led to my body experiencing an extreme transition which resulted in three severe flare-ups. My mother left Atlanta and moved back to Maryland to be closer to me because she was terrified of how sick I was getting. Each time I flared up, I flew home to get the treatment from Dr. Rosen. Suddenly, Humira no longer worked for my body anymore and Prednisone wasn’t healthy for me to keep using to reduce inflammation due to its side effects.
During senior year, my 3-week hospitalization interfered with my academics and involvement in extracurricular activities. At this time, I was advised to try Entyvio and I was tired of trying new medications. The only way I could have some quality of life was to remove my colon. My mom was concerned for me, but I couldn’t let her concerns steer my thinking I knew I had to do this for me if I wanted to make it to graduation.
In November of 2017, I set an appointment with Dr. Colvin in Northern Virginia to discuss my surgery. I had the surgery during my college winter break, spent Christmas in the hospital, recovered and returned back to school. At the time, I didn’t know how I was going to apply to graduate school at the S.I. Newhouse School of Communications at SU but I did that during my recovery period. It took a lot of exercise, mental motivation, empathy and support from family, my best friends, mentors and peers at school. With amazing grace and good spirits, I got accepted into the public relations program at the S.I. Newhouse School of Communications.
From this specific point on, learning how to function in everyday life with my ostomy took a lot of patience, time, emotional breakdowns, motivation and positive mental strength. I don’t regret any of it at all. I do not have to worry about missing out or not fully enjoying any more important events of my life. Now as of 2020, I have been medication-free for two full years, graduated school with all of my degrees, feel healthier than ever, working full-time in public relations and am actively pursuing my dreams in the entertainment (modeling/tv/film) industry.
It wasn’t until a couple of months ago, I discovered United Ostomy Association of America (UOAA) and chose to reach out to Advocacy Manager Jeanine Gleba about getting more involved. Since reaching out, I have gained the opportunity to advocate for patient’s access to treatment during the Digestive Disease National Coalition Day on the Hill and spoke on the behalf of UOAA. I am elated to have met UOAA’s team and to represent others like myself who have experienced challenging obstacles.
I couldn’t be more grateful for my ostomy and must say that it changed my life for the good. Life is full of obstacles but how you choose to overcome them will make your life. I chose to take full control of my life in order to have a better quality of life. It doesn’t matter who you are, you can truly do whatever you put your mind to. Believing in yourself and staying grounded in positivity, motivation and dedication is key. Follow your dreams, find what makes you happy and don’t let the negatives take control of your life.
The ostomy community is understandably very concerned about how the COVID-19 outbreak is affecting their daily lives, health, support networks, and access to ostomy supplies.
In this time of great uncertainty, UOAA recommends all individuals consult with their own primary care physicians with questions concerning their risk factor or if they exhibit any symptoms. Please follow the Center for Disease Control (CDC) website for actual up to date information. We recognize that many people living with an ostomy or continent diversion are older people and those with chronic disease and are therefore at higher risk of developing serious illness. Please also see CDC guidelines for people at risk.
UOAA is also hearing from many Affiliated Support Groups who have prudently decided to cancel their upcoming meetings. Members should expect that their meetings will be canceled for the foreseeable future. Affiliated Support Groups are each independently run and members should contact their local leaders if they have any questions about their meetings. Community guidelines are also available from the CDC to assist leaders in deciding steps they should take to address public health concerns.
UOAA reached out to the major ostomy manufacturers to see if the outbreak is currently impacting their production or supply chain. As of March 4, 2020 none of the manufacturers reported any issues in their operations as a result of the COVID-19 outbreak. Read our previous blog post for statements from individual manufacturers on this topic. Check with your distributor to see if there are any shipping delays due to increased demand of all goods at this time.
If you develop a fever, cough and have difficulty breathing always contact your healthcare provider. They will determine if you are a candidate for a COVID-19 test. Medicare and private insurance should cover a test to see if you have coronavirus if requested from a physician. Additionally, Medicare is offering telemedicine options so people can stay home as much as possible during this crisis. Contact your private insurer to discover any additional benefits they may be offering at this time. For frequently asked questions and facts about this virus follow updates from the CDC on the latest COVID-19 guidelines.
UOAA will update this blog post with any information that may affect our community.
By Jeanine Gleba, UOAA Advocacy Manager
The Digestive Disease National Coalition (DDNC) is an advocacy organization composed of the major national voluntary and professional societies concerned with digestive diseases. DDNC’s mission is to work cooperatively to improve access to and the quality of digestive disease health care to promote the best possible medical outcome and quality of life for current and future patients. UOAA has been a member of this coalition for many years.
Each year the DDNC hosts a Spring Public Policy Forum. This year they celebrated their 30th anniversary! This special event was a two-day advocacy conference held March 1-2, 2020 that brought together patient advocates, health care providers, and organizational members of coalition. Passionate and dedicated advocates traveled from 28 states all across the country and Washington DC. Over two days, attendees heard from multiple panels of leaders in the digestive disease community, attended a reception celebrating the coalition as well as its champions, and advocated for medical research and patient care on Capitol Hill.
UOAA had five ostomates representing UOAA and the ostomy community. We are grateful that Lacee Harper, Rena Münster, Michael Quear, Mollie Tinnin and Lynn Wolfson joined UOAA President, Susan Burns, and myself in Washington, DC. They spoke up about improving treatment for digestive diseases, shared their ostomy story and advocated for legislation such as the Removing Barriers to Colorectal Cancer Screening Act and the Safe Step Act. While mingling with attendees, we also had the pleasure of meeting a new ostomate advocate, Nancy Pedersen, and a mother of a young daughter with an ostomy, Jessi Richards, who was attending as a representative for the Megacystis Microcolon Intestinal Hypoperistalisis Syndrome (MMIHS) Foundation. We hope both of them will advocate with UOAA in the future.
 The greatest take-away message from honorees and guest panelists was the impact we make on the Hill. For example, it is truly because of patient advocates sharing their stories that we have seen increases in medical research funding. To give you a glimpse into my day on the Hill, I was on Team 6 with a surgeon from Nebraska and an IBD patient advocate from Connecticut. I found we were met with very positive responses by legislator staffers in the Senate and House. In many cases, the offices we visited were already co-sponsors of the different legislation pieces and this occurred on both sides of the aisle. They certainly all “got” the Safe Step Act and need for proper gluten labeling. When I followed up with my Congressional office (NJ Rep. Josh Gottheimer), they informed me that they have now signed on to the Medical Nutrition Equity Act (H.R.2501). Our visit and advocacy message resulted in a positive outcome!
The greatest take-away message from honorees and guest panelists was the impact we make on the Hill. For example, it is truly because of patient advocates sharing their stories that we have seen increases in medical research funding. To give you a glimpse into my day on the Hill, I was on Team 6 with a surgeon from Nebraska and an IBD patient advocate from Connecticut. I found we were met with very positive responses by legislator staffers in the Senate and House. In many cases, the offices we visited were already co-sponsors of the different legislation pieces and this occurred on both sides of the aisle. They certainly all “got” the Safe Step Act and need for proper gluten labeling. When I followed up with my Congressional office (NJ Rep. Josh Gottheimer), they informed me that they have now signed on to the Medical Nutrition Equity Act (H.R.2501). Our visit and advocacy message resulted in a positive outcome!
New this year we advocated about non-medical switching as it relates to ostomy supplies. It can take patients and their medical team quite a while to find the right “fit” ostomy pouching application system. However, we are finding for example that insurers in some cases are restricting consumers to specific brands, some suppliers switch outpatient preferred choice of products for non-medical reasons such as cost and patients are restricted to using a different brand such as a generic, which do not always have the same quality or reliability. Ostomy supplies are prosthetic devices and a person’s complete pouching system is customized for their unique stoma fit and individual needs. It is not okay for others to just switch that out! We urged Congress to limit out-of-pocket costs and curb current and future payer tactics proactively.
UOAA will continue these advocacy efforts throughout the year. If you have experienced your supplies being switched out for non-medical reasons and it resulted in restricted access to your preferred products or an increase in your out-of-pocket costs or it negatively impacted your health or quality of life, submit your story HERE.
Contact Us

United Ostomy Associations of America
P.O. Box 2293
Biddeford, ME 04005-2293
Call us toll-free at: 1-800-826-0826.
Our Information Line hours are Monday-Friday, 9am to 3pm EST. If you have an emergency, please dial 911 or contact your local medical professional.
Please understand that UOAA is a private, nonprofit, advocacy and informational organization. We are not a medical facility and we do not have medical or legal professionals on staff. Therefore, UOAA does not provide Medical, Mental Health, Insurance or Legal Advice. Visit UOAA Virtual Ostomy Clinic provided by The Wound Company for non-emergency, virtual ostomy support.
Get Involved
UOAA is the leading organization proactively advocating on behalf of the ostomy community. Recognizing that we are always stronger together, we encourage everyone to get involved by joining our Advocacy Network. We’ve also created several Advocacy Tools and Resources to help you successfully advocate on behalf of the ostomy community to ensure every ostomate receives quality care.
Latest News:
 Steve Hubbard’s Ostomy and Crohn’s StoryApril 25, 2024 - 11:25 am
Steve Hubbard’s Ostomy and Crohn’s StoryApril 25, 2024 - 11:25 am Do you speak stoma?April 4, 2024 - 2:32 pm
Do you speak stoma?April 4, 2024 - 2:32 pm Why Larry David’s “Colostomy Bag” Curb episode is making me speak out about my ostomy after 48 yearsMarch 28, 2024 - 10:43 am
Why Larry David’s “Colostomy Bag” Curb episode is making me speak out about my ostomy after 48 yearsMarch 28, 2024 - 10:43 am Osmani Gonzalez’s StoryMarch 12, 2024 - 12:20 pm
Osmani Gonzalez’s StoryMarch 12, 2024 - 12:20 pm Ostomy Advocates Taking Action in Washington, DC for Digestive DiseasesMarch 8, 2024 - 4:14 pm
Ostomy Advocates Taking Action in Washington, DC for Digestive DiseasesMarch 8, 2024 - 4:14 pm

UOAA does not and shall not discriminate on the basis of race, color, religion (creed), gender, gender expression, age, national origin (ancestry), disability, marital status, sexual orientation, or military status, in any of its activities or operations.
