Surviving colorectal cancer, reversal complications, and living with faith & perseverance
In June 2018, Osmani Gonzalez began a new exercise program to help him lose weight and kickstart a healthier lifestyle. Two months into his new routine, the then 42-year-old began to experience abdominal pain. Gonzalez assumed it was due to his workouts, but the pain foreshadowed a much more severe issue.
His discomfort only worsened over time, and in August 2018, Gonzalez, who was born in Havana, Cuba, and raised in Hialeah, Florida, was rushed to a nearby hospital with a swollen abdomen.
To alleviate his pain and to clear an obstruction in his colon, he underwent surgery for an ileostomy. During this procedure, surgeons build an opening in the abdominal wall by bringing the end of the small intestine out onto the surface of the skin, creating an opening for his intestinal waste to pass through into an ostomy bag attached to his abdomen. Unfortunately, the news that came after his procedure was not favorable – Gonzalez was diagnosed with Stage 2 colon cancer.
He cried along with his wife of 23 years Aleida, and despite not knowing what they were getting into remembers them saying, “We are going to fight it, good or bad we will try our best.”
Gonzalez thinks patients should also find time to have empathy for others. “It’s so important to understand the caregiver and ask how they are doing and to never forget that they are going through similar things,” Gonzalez says. He received 12 sessions of chemotherapy for six months. While in the hospital for treatment during the Christmas Holiday Gonzalez, who is an advocate and speaker for father engagement in K through 12 education and active in several area PTA’s where he raised two children, had an idea to bring some cheer to fellow patients by having local children draw cards of support to his fellow patients.
how they are doing and to never forget that they are going through similar things,” Gonzalez says. He received 12 sessions of chemotherapy for six months. While in the hospital for treatment during the Christmas Holiday Gonzalez, who is an advocate and speaker for father engagement in K through 12 education and active in several area PTA’s where he raised two children, had an idea to bring some cheer to fellow patients by having local children draw cards of support to his fellow patients.
Gonzalez’s cancer went into remission and was told he no longer needed the ostomy.
In February 2019, Gonzalez underwent reversal surgery. However, three days after the procedure, he woke up in horrible pain, and a CT scan revealed there was a leak in his intestine and his staples had come undone. After the blood system was contaminated, Gonzalez was diagnosed with sepsis shock and had to undergo another surgery to have an ileostomy again. Afterward, Mr. Gonzalez was put in a medically induced coma for 18 days.
“At that point, my wife was given very little hope and was told just to pray and prepare for the worst,” Gonzalez said.
When he woke up from the coma, he began occupational and physical therapies and was on an IV drip to help alleviate his constant dehydration. Gonzalez learned to walk and perform basic physical activities. He used a wheelchair for more than three months while he recovered.
Even with the support he was receiving, Gonzalez’s kidneys began to fail. During one of his many trips to the ER, a gastroenterologist suspected he was suffering from short bowel syndrome, a condition in which your body is unable to absorb enough nutrients from the foods you eat because you do not have enough intestine.
“We all have downs and need motivation. Whatever it is you grab onto, you have to have a why and decide to live.”
Gonzalez was rushed to the Hospital’s emergency department and referred to a well-known trauma surgeon and surgical critical care specialist. “He came weighing 176 pounds, and in six months, he kept losing even more weight,” Gonzales recalls the doctor saying. “We only had 125 centimeters of small intestine to stabilize him.”
For Gonzalez to get better, the Doctor placed him on Total Parenteral Nutrition (TPN) so his body could receive the nutrition needed to strengthen his intestines. Over the next two years, Gonzalez continued receiving TPN and seeing the Doctor biweekly, undergoing continuous lab work to monitor his progress.
Despite frequent challenges with ostomy leaks and TPN he would go out fishing and continued to push himself to do things he loved. He remembers one time after a shower attempting to stop an active stoma with his hand and making quite a mess, “My wife just said it’s better laughing than crying,” he recalls with a smile.
 On June 25, 2021, he was taken off the TPN and underwent a successful reversal surgery to repair his intestines, clean up scar tissue, and remove the stoma.
On June 25, 2021, he was taken off the TPN and underwent a successful reversal surgery to repair his intestines, clean up scar tissue, and remove the stoma.
On July 9, he went home with a feeding tube and by September 13, he was on a regular and independent diet. His doctor told him, “He’s been one of the most optimistic patients I have ever cared for.”
While going through this medical journey, Gonzalez had to reduce his workflow with his construction company to focus on his health. Mr. Gonzalez is currently enrolled in a program slowly allowing him to join the workforce again. He has been working in construction management and is gradually entering a more active lifestyle.
“I look at life differently now. My focus is improving daily and being more involved in my kids’ lives,” Gonzalez said. “I’m extremely grateful to the Doctor and my care team at the hospital for performing this miracle.”
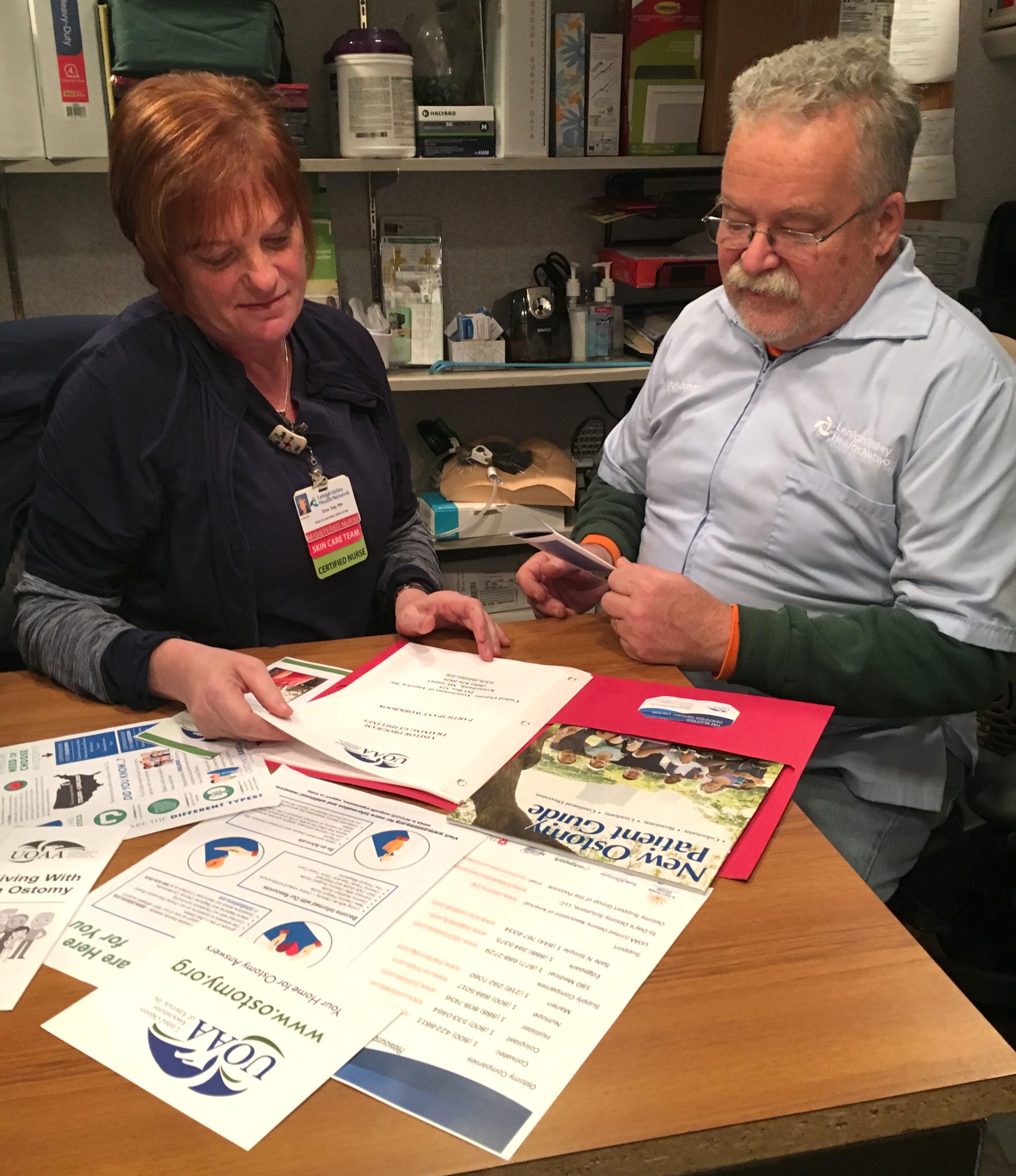
Gonzalez has expressed what a blessing it has been to have met Lynn Wolfson of the South Florida Ostomy and Tube Feeding/HPN Support Group, which provides support and comfort to other ostomy patients and guides patients through their journey of living with these conditions.
Gonzalez recently had the chance to share his story with the group and UOAA followers around the country on a Zoom presentation. He stressed the mental aspects of recovery and looking beyond day-to-day challenges.
“Keep pushing and do what you love, sometimes even when you don’t want to do something, once you start the process your feelings change,” Gonzalez says. “We all have downs and need motivation. Whatever it is you grab onto, you have to have a why and decide to live.”


 Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary
Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary 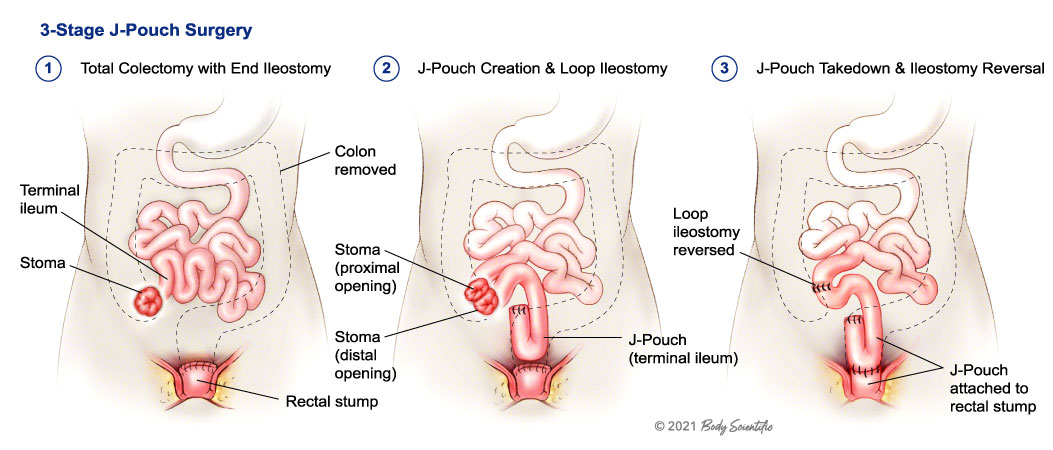
 another proud scar.
another proud scar.