Expect More – Take Control of Your Health Care
Part 3 in Series
By Jeanine Gleba and Keagan Lynggard-Hysell
The Choice is Yours
Having the right ostomy supplies for your individual lifestyle and stoma type plays a huge role in the quality of your life. As a new ostomate I fell victim to the common misconceptions that daily leakage and skin irritation were normal occurrences that came with the territory of having an ostomy, when in reality I was going through unnecessary struggles due to the fact that I wasn’t using the best products for my individual situation.
For those unfamiliar with my story, shortly after my diagnosis of Crohn’s disease in 2005, I was rushed to the Emergency Department with a bowel perforation and underwent my first ostomy surgery. After the operation, I endured many complications due to several different infections and the severity of my disease. I was hospitalized for a consecutive 8 months and would face 5 more surgeries within that first year of my diagnosis, all resulting in either a colostomy or ileostomy. Being in the hospital for essentially the first year of having a stoma, I was limited to the ostomy supplies provided by the hospital. Once I made the transition home and was receiving home health care I continued using the same supplies I had been using in the hospital simply because it was all I had ever known.
For the first few years of living with my ostomy I was isolated by the insecurities fueled by daily pouch leaks, chronic skin irritation, and the fear of experiencing a leak or unexpected odor in public. It wasn’t until I got to the point where my peristomal skin was so excoriated and I could no longer keep a pouch on for longer than a few hours that I finally made an appointment to see a WOC nurse.
During my appointment, not only were my skin issues addressed, but my WOC nurse introduced me to a new ostomy appliance and accessories that would work best for my individual stoma and lifestyle. I was given a product catalog which my WOC nurse had marked with tabs on the new products we used that day so I could order them for the upcoming month as well as any samples of other supplies I was interested in trying in the future. That day, I left my appointment feeling comfortable and confident in my new ostomy appliance.
As time went on, I no longer experienced the daily leakage or skin irritation that I had with my previous appliance, and this drastically improved my quality of life. I was no longer worried about odor, or ruining my clothes, I felt more confident in public and was able to participate in the activities I had once restricted myself from doing out of fear that my ostomy appliance would not stay on properly.
As ostomates, we are fortunate that manufacturers continue to improve our ostomy supplies. For the last 13 years that I have been living with my ostomy I have benefited greatly from product innovation and feel confident in the ostomy appliance I wear today.
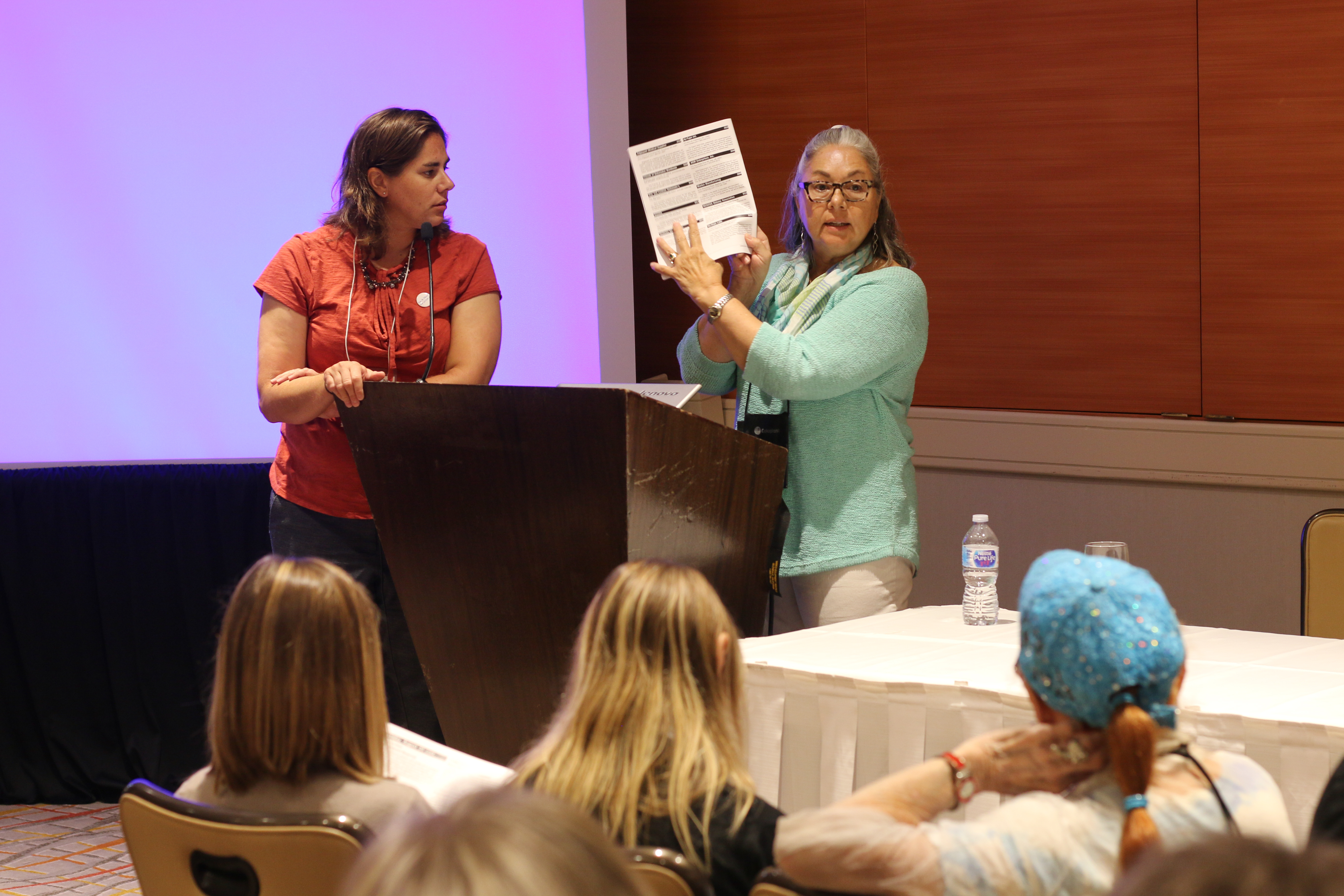
As an ostomy patient advocate, I am often invited to share my story with nursing students, WOC nurses, as well as other health care professionals. By providing the patient perspective, I encourage them to educate their patients on the supply options available and that a patient’s ostomy appliance plays a huge role in their everyday life.
It’s important to remember that our stomas may change, our bodies may change, and more often than not- our ostomy supplies may change- and that is okay! The most important thing to remember is to seek out the most optimal pouching appliance for you so that you may live the life you love and want to live. The most important thing to remember is, whatever works best for you and your individual stoma.
Know that you have Ostomy Product Choices
As listed in the UOAA Patient Bill of Rights, ideally before patients are discharged from the hospital they should be informed of the pouching system that has been prescribed to them as well as have an understanding of the ostomy supply ordering process. In addition to the pouching system prescribed, patients should be provided with information on the supply choices available to them once they are home.
When in the hospital, your ostomy supplies are included as a part of your treatment of service. To keep costs down, the hospital only has a small selection of ostomy products from a particular manufacturer vendor that they contract with. As a result patients are initially limited to whatever ostomy supplies the hospital uses. Know that you are not locked into any pouching system and that you have many choices to find the ideal system for your stoma and lifestyle. (It should be noted that many patients stay with their initial hospital brand and are very satisfied with these supplies.)
Before you leave the hospital be sure to get the product codes for the specific ostomy supplies used while in the hospital. Request that extra ostomy supplies be sent home with you upon discharge to ensure you have enough on-hand until your first order arrives at home, or until your first home nurse visit if you will be receiving home health care. Don’t forget to ask about being enrolled in one of the discharge programs that are sponsored by ostomy manufacturers.
It is completely normal for your stoma size to change in the weeks following surgery, so what was initially prescribed in the hospital might need to be altered.
As always it is strongly encouraged that you work with an ostomy nurse to find the best products to meet your needs and particular situation. Manufacturers’ also have WOC nurses available to discuss any issues or answer your questions if you do not have a WOC nurse/OMS available in your area. Their services are free of charge and they are dedicated to helping you.
When you are ready, feel free to experiment with different manufacturers or different types of products. It may be helpful to order a product catalog from your medical supplier, so you can see the different products available and what assortment you have to choose from. Also, either you or a family member can call the manufacturer’s toll free 800 number and request product samples, or ask your supplier for a sample.
Know Your Pouching System
In the ostomy world, it is wonderful to know that there are many different styles and types of pouching systems available, and that manufacturers are continually improving their styles and selections. Manufacturers listen to ostomy nurses and to patients as they seek to improve the lives of ostomates.
It is good to understand the basics of pouching systems and then advance your knowledge as you become familiar with your own system. Once you gain confidence in the terminology, you can begin to explore options for yourself. Please use this link to learn about the different types of options available. Another excellent resource is here.
Know Supplier Options
The major manufacturers do not sell supplies directly to ostomates. Furthermore, ostomy supplies are rarely available for purchase in chainstore pharmacies such as CVS or Walgreens. Before you begin ordering ostomy supplies, itis important to do your research (read online reviews too) and carefully consider your options when choosing your supplier (Under Medicare these are known as Durable Medical Equipment providers.). Some things to consider when choosing your supplier: affordability (reasonably priced), reliability (on-time delivery) and reputation (quality service). You should also know the answers to these questions before deciding on your supplier:
- Do you want to shop at and support a small local medical/surgical supply house or order from the convenience of home through a large mail-order house (aka national online vendor)? There are pros and cons to each but typically national vendors carry a wider range of products, many (but not all) accept Medicare assignment and due to higher volumes can offer lower pricing.
- Do they accept your health insurance?
- What are the prices before and after your deductible is met?
- Do you have to submit the claim for reimbursement to your insurer or do they directly bill the insurance company for you?
- Do they carry all of the products that you need for your unique pouching application system?
- Do they stock and keep current with the latest available in ostomy technology and do they suggest new products?
- If you are on Medicare, do they “accept assignment”?
- What is the return policy or how do they handle product issues such as defects or incompatibility?
- Do they only ship in quantities for 30 days (1 month) or also offer 90 day (3 month)?
- Do they charge shipping?
- Do they impose their own quantity limits on supplies?
- How long does it take to receive orders?
- Do they help rectify insurance denials and work on appeals?
- Do they work with your doctor to renew your prescription or if you need a change to your supply order?
- Do they have personalized customer service with helpful reps knowledgeable about ostomy supplies?
- Do they offer free ostomy nurse consultations to give you tips and guidance?
Tip: Be sure to have a back-up supplier in case your normal provider has a disruption in service or is waiting for your type of supplies on back-order.
Know what Information is Needed to Order Supplies
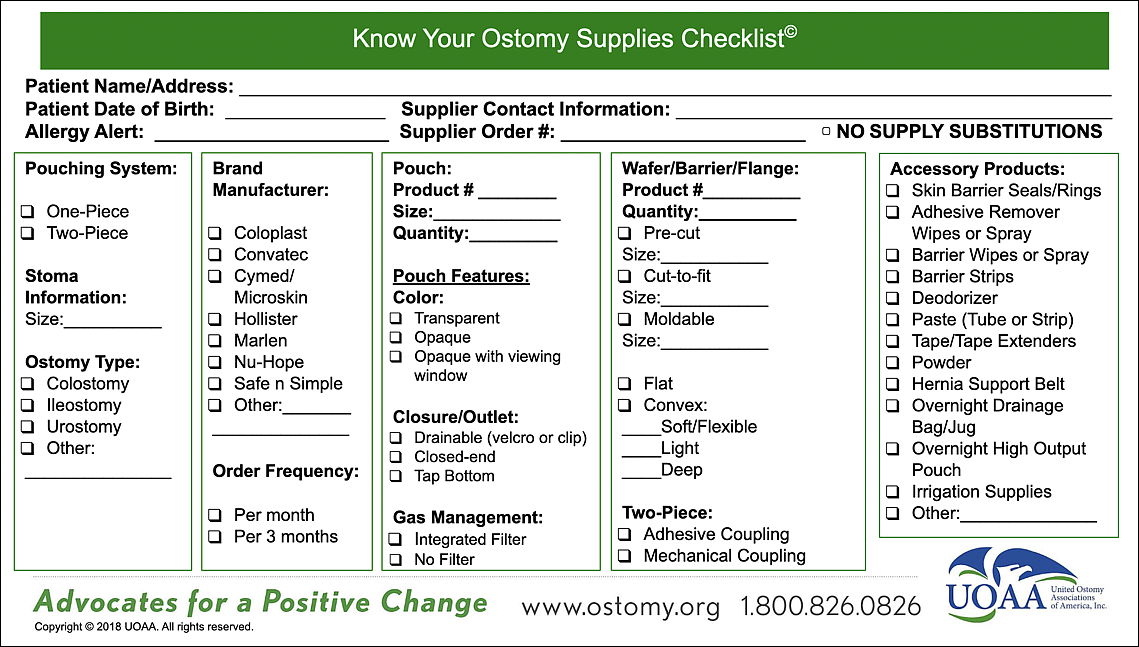
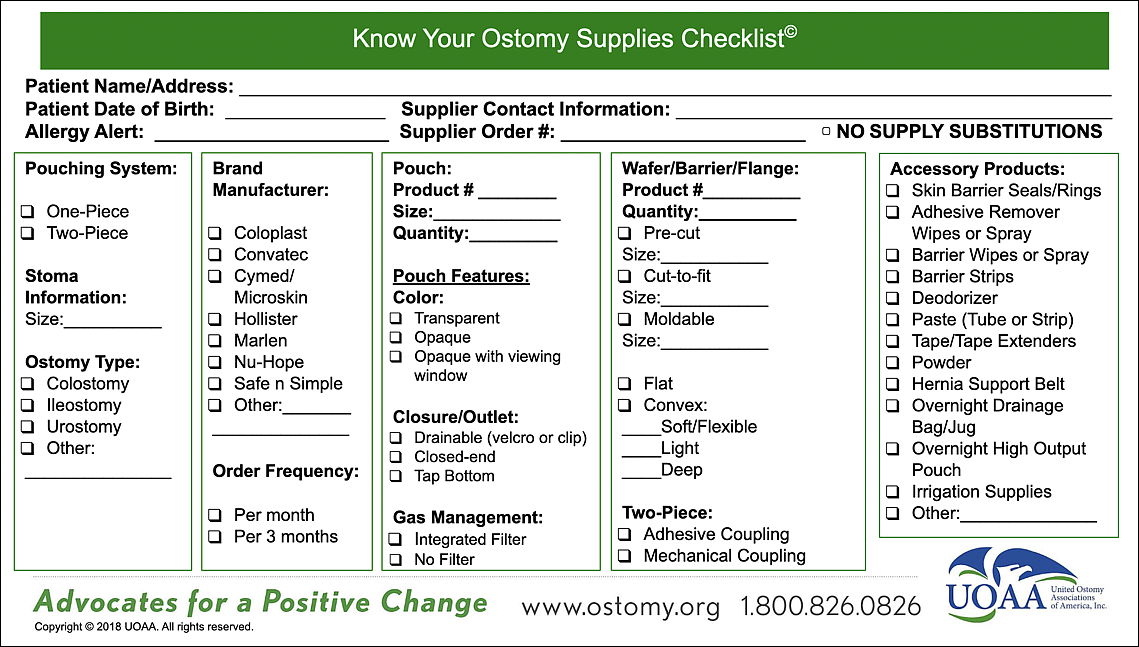
It’s helpful before you place an order to have all of the information about your pouching application system ready. The most important thing to know when placing an order is the order number for your particular supplies and accessories. The order number will tell the supplier what kind of pouch and accessories that you use. If you are ordering for the first time or switching suppliers, be sure to know the type of ostomy appliance and any other accessories that you use. Include the pouching system product, size, and product number. Download the UOAA Know Your Ostomy Supplies Checklist tool to have handy.
Conclusion
Knowing your current ostomy appliance and accessories, where and how to purchase them, that options are available in product selection, and that you have a choice in all of these decisions helps to make you in control of your ostomy health care. In addition, utilizing the resources available to you through your ostomy manufacturers, suppliers, and ostomy nurses will help provide the best experience with your supplies.
It is important that you are able to advocate for the right ostomy supplies that work best for you and your individual stoma so that you can feel confident and live well with your ostomy.
Please note: UOAA does not endorse particular products, manufacturers, or suppliers, and is not responsible for any content expressed in sponsor websites.


 Wow. Right?
Wow. Right?