Ostomate or Person Living with an Ostomy?
“Labels are for soup cans.” ~ Grist Mill Road by Christopher Yates
by Jeanine Gleba, UOAA Advocacy Manager with Keagan Lynggard, UOAA Advocacy Committee Member
The UOAA Advocacy Committee produces many educational resources and self-advocacy tools for the benefit of you; you being a person living with an ostomy or continent diversion. Our dilemma has been what to call you or how to refer to you within the context of advocating, educating, and supporting, as you are the subject of what we write about. Sometimes we call you “a person living with an ostomy or continent diversion”. That takes nine words to describe one aspect of your life and this becomes very difficult and cumbersome to write over and over again in a single advocacy or educational document. There is however, a definite trend on social media and with online bloggers to use the word “ostomate” when referring to you, and the community of people who live with an ostomy.
As a national organization that supports all people living with an ostomy it’s crucial that we are sensitive and choose our words wisely so that they are acceptable to our community. Ostomy surgery is already a delicate topic that is often associated with “bathroom talk”, a topic that already has enough of its own societal taboos. Recently our Committee set out to gather survey data to hear from YOU, the people that our work impacts to identify the more acceptable or best term to use in our advocacy written materials and presentations concerning ostomy awareness and education.
Is this a label?
Our surveys certainly sparked an interesting debate. Many responders assumed that we wanted to “label” our community in a derogatory way versus our intention which was to simply look for a word to identify our medical demographic and represent the people we impact. As I read the comments from our responders and thought about what we were looking for, it made me wonder if this is how “labels” are born? Do they arise when people search for a simple and easy to use term to describe something? What happens when a label sticks and there is a negative stigma or insensitivity to those with a particular condition? As I pondered these questions and continued to review further comments, I realized that many people do prefer a simple word (or label) to identify their medical condition. It helps some people feel a sense of belonging and unity within a unique group. So I’m not sure what we would even call the word: a “term” or a “name” or a “label”? It’s also important to stress that although we were looking for a simpler non-offensive term it wasn’t meant to completely and irrevocably replace a “person living with an ostomy”. In fact, the definition of the word “ostomate” is simply a person who has undergone an ostomy.
And the preferred term is…
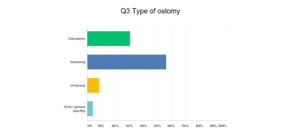
Here are the results of our surveys:
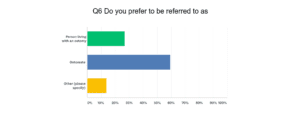
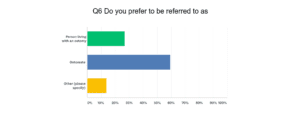
Total Votes: 331
34% (113 votes) Person with an ostomy
61% (201 votes) Ostomate
5% (17 votes) Other
191 Votes via Facebook
37% (71 votes) Person with an Ostomy
63% (120 votes) Ostomate
23 Votes via Twitter
48% (11 votes) Person with an ostomy
52% (12) Ostomate
117 Responses via Survey Monkey
27% (31 votes) Person with an Ostomy
59% (69 votes) Ostomate
14% (17 votes) Other
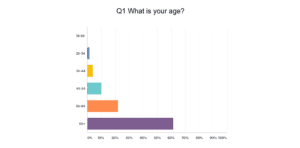
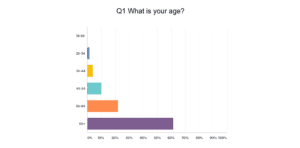
Does age affect preference?
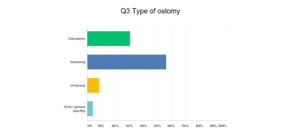
In the Survey Monkey survey we asked a few more questions to gain a better understanding of the responders, such as gender, age, or whether their ostomy was temporary or permanent. 98% of the responders had a permanent ostomy with over 80% being older than 55 years of age. Of this older population 62% were female and 38% were male. Of interest the males were 50-50 in their selection of preferred term. Whereas, only 17% of females preferred “person with living with an ostomy”. If this had been a science experiment, and I had to develop an initial hypothesis, given the social trends on the internet, I would have predicted that the term “ostomate” was going to be more favorable for the younger generation. Our results proved this wrong!
We also provided an opportunity for people to list a specific “other” term that they would prefer and only three had a specific response like “Packin’ a Pouch”. For the majority of those who selected “other” they did not list another term but rather said it was actually ok to use “ostomate” or they didn’t care, which in turn would increase the # of who prefer “ostomate”. Nineteen percent (3/16 responses) did not want any term.
For the question “For those who do not like the term ostomate, why?” these were some of the reasons why:
· Because I am more than my ostomy or my ostomy doesn’t define me
· Labels what/who you are
· People won’t know what ostomate means or it always needs more explanation
Until you walk in someone else’s shoes…
Here’s what people were saying:
“I don’t want to be defined by my ostomy. Giving me a title/name defines me. I am a mother, a wife, a nurse, and a friend. Those things define me. Not my ostomy. While my ostomy is a part of my life, it does not define my life. PLEASE get away from the term “ostomate.”
“I prefer to focus on the positive – I am LIVING with an ostomy. Ostomate sounds harsh.”
“I also like “Person living with an ostomy”, but Ostomate is easier. What I really don’t like is use of the word “bag” which many, many people, ostomates, nurses and doctors continue to use. It’s very upsetting!” (Check out the Vegan Ostomy blog on this topic.)
“This term is commonly thought to be someone with a bowel ostomy. Mine is an urostomy. I’d like to see a term implies all ostomies.”
“Living with an ostomy sounds better to me and denotes the fact the ostomy gives a person additional life.”
“It labels people (similar to how one would not want to be referred to as the amputee, the diabetic, the bipolar, etc.)”
“I am not a “joiner” and do not plan on meeting others with similar conditions.”
Of notable interest 16/55 people answered this question with a response that they actually like the term ostomate.
In general our overall analysis found that although we did receive a few “neither” or “either” comments followed with the pattern of commentary along the lines of “my ostomy does not define me”, the vast majority preferred the term “ostomate”. We also received comments that support the idea that those who prefer the term ostomate are those familiar with the literal definition of ostomate, those who are involved/active within the ostomy community, or those who have really embraced this aspect of their life. This sense of community was evident in the survey question showing over 70% of responders belong to some sort of support community either online or an ostomy support group.
There is no right answer.
In conclusion, the Advocacy Committee has decided that in most cases we will continue to use the terminology “person living with an ostomy”, which is less “defining”, in our materials; however, given the results of the survey we will also now more freely and confidently include the term “ostomate” in order to simplify a document or when the term is more suitable for our advocacy purposes. I believe in our society of political correctness, we will never be able to please everyone, but we should always aspire to do our best, be respectful of all and try not to stir the pot by adding salt to wounds that are in the process of healing.
Thank you again to all those who participated in the survey and contributed to helping us gather this valuable information.


 Wow. Right?
Wow. Right? After eight years of not responding to western pharmaceuticals, at the age of thirty, I found myself facing a colectomy. While I had anxiety about the ostomy surgery and fear of the unknown, my overall emotion was relief. This surgery was hopefully going to be the end of many years of pain and suffering. Thanks to the encouraging words of other ostomates I was wheeled into surgery with a smile on my face, excited about what the future would hold for me–I saw endless possibility!
After eight years of not responding to western pharmaceuticals, at the age of thirty, I found myself facing a colectomy. While I had anxiety about the ostomy surgery and fear of the unknown, my overall emotion was relief. This surgery was hopefully going to be the end of many years of pain and suffering. Thanks to the encouraging words of other ostomates I was wheeled into surgery with a smile on my face, excited about what the future would hold for me–I saw endless possibility!