Give to Make an impact in the ostomy community
Your support makes a difference in so many lives. People often turn to UOAA in times of concern and uncertainty. UOAA’s staff and volunteers provide assistance every day to people across the country who are seeking knowledge, resources and support as they navigate their way through living with an ostomy. Your donation to our mid-year campaign will ensure UOAA will continue to be a trusted resource for caregivers, family members and medical professionals. Please help us reach our fundraising goal of $110,000 this year.
“Thank you for all your support. Probably without my local support group and UOAA, I seriously doubt I would have been aware of a WOC nurse or a method to receive the medical treatment I thought was necessary. Now…I will be able to live a healthier, productive life.” J. R.
General Fund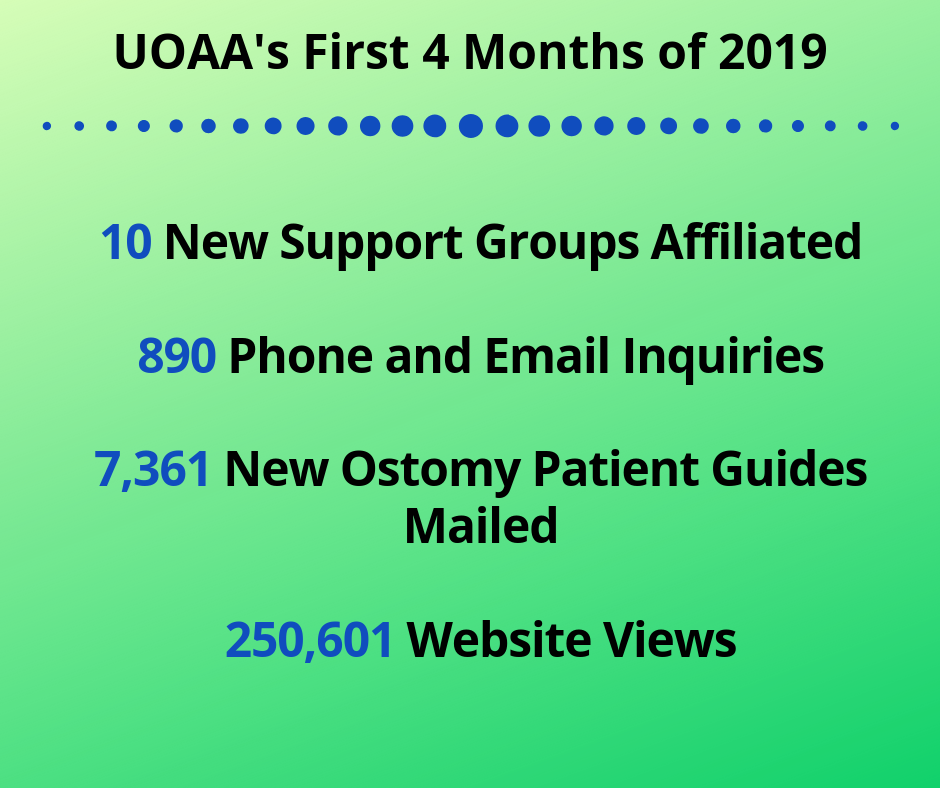
Support UOAA as we continue to create and share our educational materials, connect people to affiliated support groups, maintain our informative website and engage with medical professionals who care for the ostomy community.
“I appreciate the support of UOAA. We use the website in the clinic as our major resource and the booklets are great for the staff in-services. I have given copies to the medical students when I give the ostomy lecture during their trauma rotation as well…” C. C.
Advocacy Fund
Your financial contribution will help engage UOAA and its Advocacy Network (over 650 supporters) in legislative advocacy efforts.
“Just want to tell you what a wonderful advocacy tool you have provided to ostomates and affiliated support groups around the country…I can appreciate how the product of your work will encourage individuals and groups to move ahead with advocacy.” P. M.
Ostomy Awareness Fund
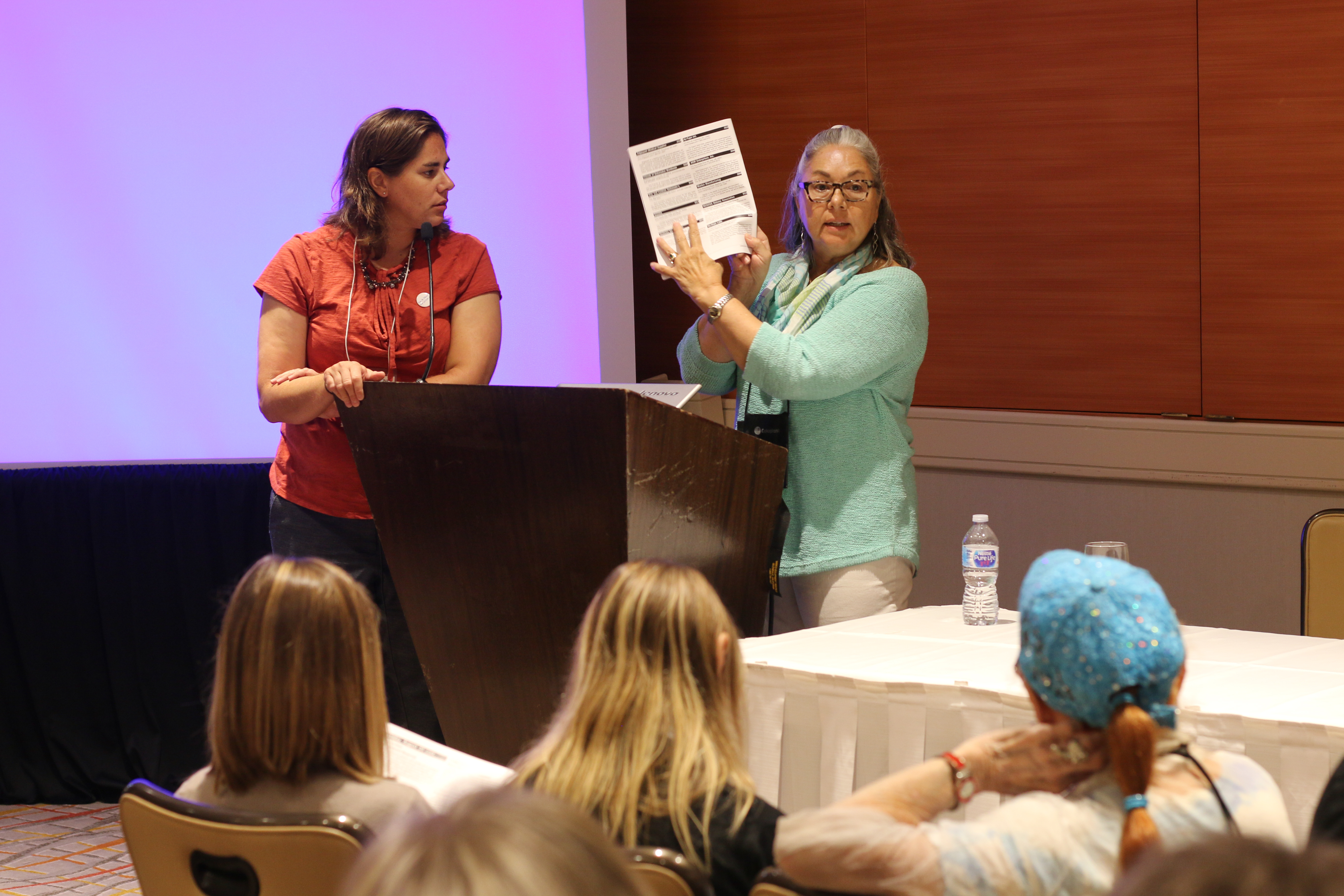
Assist UOAA in dispelling the fear of undergoing this life-saving and life-restoring surgery. Attendees of our biennial conference (join us August 6-10, 2019 in Philadelphia) have the opportunity to learn from top medical professionals, network with fellow ostomates and share their life experiences.
“Keep up the good work! I have had an ileostomy since 2002…I am retired and now perform at festivals and enjoy life! Life begins at whatever age you shake off your fears and decide to fulfill your reason for being!” K. T. H.
With your donation we can empower people living with an ostomy or continent diversion, promote quality of life, and continue our work to erase the myths and stigma surrounding this life-saving surgery. Together we can change lives.
Sincerely,
Susan Burns
UOAA President
Click here to donate today or learn more. United Ostomy Associations of America, Inc. (UOAA) is a 501(c)(3) charitable organization and all donations are tax deductible. UOAA has a GuideStar Gold Seal of Transparency.



 Support Made the Difference Before Reversal
Support Made the Difference Before Reversal
 Wow. Right?
Wow. Right?