Tag Archive for: leaks
By Robin Glover
Oh no! An ostomy! You’re going to be pooping or peeing into a bag attached to your stomach?? Your life is over, right? No more dating. No one will ever like you. Children will run from you! It’s so gross!
Don’t worry. We’ve all been there. As great as they can turn out to be, the idea of getting an ostomy is never really welcomed news. Add on to that, you’re probably very sick and haven’t eaten well in weeks and you’re tired and worried and feel alone. You know nothing about ostomies and are wondering what life will be like with one.
Will having an ostomy bag eventually become second nature and you won’t even really think or worry about it? Yes.
First of all, life is going to be great! You’ll feel better. You’ll eat better. You won’t be bleeding out of unspeakable places and constantly panic-stricken about finding the nearest bathroom. Your life will become more consistent and routine and you’ll end up being happy you had a lifesaving, life-improving surgery.
It’s possible that you don’t believe that right now, though. And while it does turn out to be a good thing for most, there is an adjustment period and a lot of unknowns and myths. For instance, how do I change my ostomy bag? Will I stink? What if I have an accident in public? Can I ever play sports again? Or exercise? Or go swimming?
In short– is it easy? No. Will it be fine? Yes, yes and yes. But for a little expanded information and peace of mind, we can go into a little more detail.
How Do I Change My Ostomy Bag?
You gently peel it off, wipe things off a bit, and put another one on. It really does become as simple as that. But, at first, you’ll hopefully have a specialized ostomy nurse that will teach you how to do it. After your surgery, you likely won’t have to change it yourself the first several times. But, you should practice doing it and will be better off if you make the effort to know how before you leave the hospital. It also helps to know what the standards of care should be for ostomy patients and speak out before you are discharged and sent on your way.
If you did not have access to a certified ostomy nurse in your hospital be sure to seek one out. You can also find a Wound, Ostomy and Continence (WOC) Nurse or an Ostomy Management Specialist (OMS) through product manufacturers and telehealth services.
Will My Ostomy Bag Leak?
At first, Yes. It likely will. You might even get really frustrated in the beginning because you can’t seem to put it on as well as the nurse in the hospital. Even if you put it on “perfectly” and follow all the steps your ostomy pouch can still leak. You’ll get the hang of it, though. Every ostomy and everybody is different. You’ll learn what supplies you need, where to get them, and how to use them to make sure the fit is just right.
While you might be hesitant to leave the house for a while, you’ll soon feel totally confident going anywhere you want, any time you want. And better yet? You won’t be constantly worried about being near a bathroom! There’s always the risk of a leak, though. But it won’t be a big deal. You’ll be able to detect it quickly and take care of it.
Will I Smell?
No. If the appliance is attached correctly, you should never stink. No one will be able to smell you. You can be as close as you want to other people. You can go out and be in a crowded bar and nobody will know you have an ostomy bag. There are also plenty of clothing and garment options to fit well with your pouch and conceal it from anyone ever knowing – if that’s how you choose to approach it.
If you do ever smell, that means you need to check your pouch for any leaks or openings allowing odor to escape. And if you happen to be in public, you can carry tape or any of a variety of things to sneak off into the bathroom and do a quick fix. Will it be uncomfortable or scary the first time it happens? Yes. Will having an ostomy bag eventually become second nature and you won’t even really think or worry about it? Yes.
(Quick note: The answer to a lot of questions about having an ostomy is that “you’ll figure it out” or “you’ll become comfortable” because everything will be new when you first have an ostomy bag. There’s no step-by-step guide. There will be frustrations. Maybe some tears. It’s an adjustment. Nobody just has ostomy surgery, learns to put on a pouch, and then goes about their business. You will have issues. You may have some stained clothes and probably need to change your bedsheets one or two times. But, you will figure it out.)
Can I Do Whatever I Want?
Generally speaking, yes. Of course, this depends on every unique situation, and only you and your doctor can accurately answer this question. But, in general, you’ll be able to do whatever you want. Simply having an ostomy won’t restrict you from doing anything. You might even be able to do a whole lot more than you could before.
You’ll be able to go swimming, play rugby, do mixed martial arts, teach yoga, travel the world, go on dates, and do anything you were physically capable of before having surgery. All without worrying about being in constant pain or eating the wrong thing or needing to run to the bathroom every five minutes. However, make sure to wait 6-8 weeks or until your doctor approves you for any strenuous physical activity before winning the local 5k again. (Perhaps you’ll even want to take part in UOAA’s own Ostomy 5k.)
Getting An Ostomy Is Totally Worth It
All the details about how to change your ostomy pouch where to get supplies, and when you can go back to doing the things you love will get worked out. But the important thing to remember is that having ostomy surgery is going to be totally worth it. Even if your head is spinning now about what life will be like, it will calm down.
And also remember that you’re not alone. One of the best ways to prepare is to call or visit an ostomy support and information group before you have surgery. Many others have been through the same process and are more than eager to offer a listening ear and emotional support. UOAA also offers a new ostomy patient guide and has tons of online resources to get you started on the right path.
You’ll get the hang of everything, then look back and be so grateful that you are a warrior. Countless other ostomates will tell you the same thing. That is, when they’re not busy living an incredible life they wouldn’t have otherwise.
You got this!
Robin Glover is a writer based in the Houston area. He has a permanent ostomy after being diagnosed with Crohn’s Disease in 2017.
Sponsored by Coloplast
Have you ever experienced skin issues under your barrier? While peristomal skin conditions are all too common, many are easily treated – and better yet, avoided – with the right knowledge, product fit, and support. Finding the right ostomy barrier to fit your individual needs can be a challenge and may involve trying a few different barriers to fit your unique body and stoma. Getting a nice snug fit between your stoma and ostomy barrier is key to protecting your skin, and helps you reduce the risk of experiencing a frustrating cycle of stoma leakage and resulting skin issues.
If you see an ostomy nurse – great! Every person’s situation is unique, so if you’ve worked together on a solution, or if you’re currently experiencing skin issues that may require a specific intervention, I highly recommend working with your ostomy nurse to find the routine that works for you. That said, below are some general tips that are relevant to anyone with an ostomy.
As the saying goes, “An ounce of prevention is worth a pound of cure” – meaning it’s preferable to take precautions than to suffer the consequences later. This is also true in ostomy care. So, what can taking precautions for peristomal skin health look like? While it may not be realistic to prevent skin issues 100% of the time (after all, things happen!) finding a well-fitted and comfortable pouching system for your stoma and body profile is a great place to start in reducing your chances of skin issues. I always like to explain proper fit like trying on shoes at the store. When buying a new pair of shoes there are different criteria to follow. For example, is this the right size? Is it too big? Too small? Does my foot move around too much or not enough? Does it chafe when I bend too much or too fast? All these questions can also be asked when selecting the fit of your ostomy barrier.
The right barrier?
While you might sacrifice comfort for a number of reasons when you’re picking a new pair of shoes, your ostomy barrier should be treated more like your favorite go-to shoe no matter the occasion – going out on the town, running on the trails, or enjoying a quiet night in. If your shoe doesn’t fit and move with your foot just right, you may find that you have blisters on your heels from walking in them for too long. Similarly, if your barrier doesn’t move with your body while you sit, stretch, and go about your day, you may also find blisters or painful sores underneath your adhesive. That’s why the adhesive of your product is also important to consider when finding the right barrier for you – there are a lot of options out there! For instance, there are options for more stability around your stoma, more flexibility, special sizes and shapes to better fit your body’s contours, more resistance to breakdown from stoma output, and a host of other options that your WOC nurse can help you navigate. No matter which option you choose, an ostomy barrier should move comfortably with your body and shouldn’t limit your activities or range of motion.
Does this fit just right?
A great question! Let’s continue referencing trying on shoes. If the shoe is too large, your foot slides around and can create some friction in some places like your heel or your toes. Ouch! If the shoe is too small for your foot, it’s too tight and is quite uncomfortable, which can also create some friction and maybe some sores, much like when the shoe is too big. So, how do we relate this to an ostomy barrier? Let’s discuss! An ostomy barrier needs to be snug to the stoma and measured properly. If the barrier size is cut too big, the risk of stool or urine on the skin from the fit not being appropriate can create irritation or even sores. If the barrier is too tight, the proper seal may not be achieved, and the improper fit could lead to irritation on the skin or even to the stoma if the fit is far too tight. Just like you would use a previous shoe size as a reference or a foot-measuring size guide at the store, utilizing a stoma measuring guide to size up your stoma may be key to getting the right fitting barrier. You want to make sure that the measuring guide fits snug around the stoma, but not too tight, and just close enough to the stoma so the skin doesn’t show through.
For illustration purposes only. Performance and experience may vary. Talk to your healthcare professional about what may be right for you. Please refer to product ‘Instructions for Use’ for intended use and relevant safety information.
What is a solution?
Finding the right solution may take a few tries to find the right fitting barrier for your body type and your stoma size. When finding the right fit, the goal is to reduce any peristomal skin irritation or issues you could experience from improper sizing. Utilizing a size guide or template that you created is helpful with each pouch change to stay consistent. If the fit of your barrier changes, like after surgery when your stoma swelling goes down, creating a new template may help reduce potential peristomal complications.
Making a routine for fit
Don’t forget to do a body assessment when you perform a stoma assessment. What is a body assessment? Let’s reference shoes again. Just like when you try on a pair of shoes from many years ago that used to be your favorite to wear, you may find that when you try them on, they no longer fit, and it’s time to go up a shoe size. Similarly, it’s important to observe your stoma and skin over time to make sure that the barrier you’re using still fits right. All bodies change over time, especially our skin. Fluctuations in weight and differences in skin texture may impact the fit of your barrier. One way to stay on top of your body assessments is to do an online check. Coloplast’s BodyCheck tool is a simple way to check in on your fit and assess your body and stoma profile. If you feel it has been a while since the last time you checked in with your WOC nurse for a barrier fitting, I’d certainly recommend scheduling an appointment, too. Current guidelines recommend an annual checkup with a WOC nurse, and this is a great way to get back on track with your fit.
 Mackenzie Bauhs, CWOCN, is currently an employee and Ostomy Clinical Consultant for Coloplast. She obtained her bachelor’s degree at Carroll University in Wisconsin. She has worked with ostomy patients in the post-operative period at the University of Wisconsin Hospital and Clinics in Madison, Wisconsin as well as outpatient ostomy care at Rush University Medical Center in Chicago, Illinois.
Mackenzie Bauhs, CWOCN, is currently an employee and Ostomy Clinical Consultant for Coloplast. She obtained her bachelor’s degree at Carroll University in Wisconsin. She has worked with ostomy patients in the post-operative period at the University of Wisconsin Hospital and Clinics in Madison, Wisconsin as well as outpatient ostomy care at Rush University Medical Center in Chicago, Illinois.
The materials and resources presented are intended to be an educational resource and presented for general information purposes only. They are not intended to constitute medical or business advice or in any way replace the independent medical judgment of a trained and licensed physician with respect to any patient needs or circumstances. The information presented or discussed may not be representative of all patient outcomes. Each person’s situation is unique, and risks, outcomes, experience, and results may vary. Please see complete product instructions for use, including all product indications, contraindications, precautions, warnings, and adverse events.
Editor’s note: This article is from one of our digital sponsors, Coloplast. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.
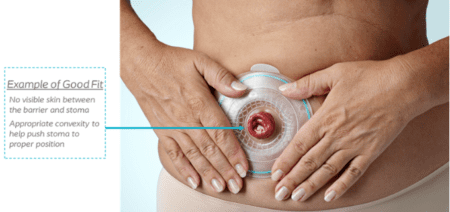
A convex ostomy skin barrier can help prevent output leakage and skin issues. Unfortunately, some misconceptions about convexity may keep people with ostomies from using it.
A convex pouching system refers to the shape of the back of the ostomy skin barrier – the side that goes against your skin. A convex skin barrier is not flat, rather it is curved or dome shaped. Using an integrated convex skin barrier is often referred to as “adding convexity” to a pouching system. This convexity provides a gentle push on the belly, allowing the stoma to protrude up and outward. This can help output go directly into the pouch and not under the skin barrier (which can cause a leak).
Common reasons for using convexity are to prevent leakage and related skin issues, and to avoid having to change the pouching system more frequently. If your pouching routine or body weight has changed, chances are it’s time to consider using a convex skin barrier.

Flat Skin Barrier

Convex Skin Barrier
Below are a few myths or misconceptions about using convexity:
- All convexity is the same
Convexity should be chosen and customized based on your specific stoma and body shape. There are two main types of convexity: soft and firm. Soft convexity is flexible and conforms to your body as you move. Firm convexity is rigid and provides firm support around your stoma to help it stick out. In most cases, soft convex skin barriers are used on firmer abdomens, and firm convex skin barriers work best on softer abdomens. Someone may have a bad experience with convexity, only to learn that it was the wrong type for their stoma, body shape, or output. It’s important to know that the convex skin barrier opening needs to be close to the stoma in order to help the stoma protrude. This will also help reduce the possibility of leakage.
- A convex skin barrier is uncomfortable or even painful
If your convex skin barrier is causing pain or discomfort, you are not wearing the right type of convexity. Based on your needs, and with guidance from a healthcare professional, consider trying some of the many convex barrier options available and see if they make a difference. The importance of addressing leakage should outweigh the fear of trying something different. Use the health of the skin around your stoma as a barometer. If your skin looks good, and you are not leaking, you’ll know you’re using the right type of ostomy skin barrier for a good fit.
- I have to wait to use convexity
You don’t need to wait a certain amount of time before using a convex skin barrier. Each person is different. Some may need to add convexity immediately after surgery, while others may not need to add it at all. There is no concrete rule, and it depends on the type of stoma you have and how well it protrudes. If your belly is soft enough, you can start right away. Again, it’s important to prevent leakage while keeping the skin around your stoma healthy, and trying convexity could help accomplish both goals.
- If my stoma is level with my skin, I need a convex skin barrier
In most cases this is true, but choosing a type of convexity can depend on your stoma output. There are always exceptions and everyone has different experiences. For example, someone who has a colostomy with formed stool and regular bowel habits may not need to use convexity, even if their stoma is flush to the skin. That’s because formed stool is unlikely to leak underneath the skin barrier. On the other hand, more liquid output can increase the chances of leakage.
Consider trying a convex ostomy skin barrier to see if it will help prevent leakage and skin issues, and increase your pouching system wear time (i.e., how long you can wear your skin barrier before it fails). Convex skin barriers come in both pre-cut and cut-to-fit options and are covered by most insurance plans. An ostomy nurse can help determine which type of convexity is right for you and when you should use it.
For more information on skin barrier convexity and other resources, visit the Hollister Ostomy Learning Center.
Terri Cobb earned her RN degree in 1991 and became a board-certified CWOCN in 2011. Currently on staff at the Cleveland Clinic in Cleveland, Ohio, her responsibilities include caring for ostomy patients of all age groups from the neonate and beyond. Terri interacts with patients in all phases of their journey from pre-op, to immediate post-op and through follow-up care. Financial Disclosure: Terri received compensation from Hollister Incorporated for her contributions to this article.
Editor’s note: This article is from one of our digital sponsors, Hollister Incorporated. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.
Two ostomy community leaders discuss effective ways to stay positive when times get tough.
Living through a crisis is hard for anyone, but there is an extra layer of concern for people with ostomies. Hollister sat down with two influential people in the ostomy community to find out how they cope during challenging times.
Amber Wallace is the creator of the Ostomy Diaries YouTube channel and social media platforms, and Dr. Paul Wischmeyer, MD is a critical care, perioperative, and nutrition physician at Duke University School of Medicine in Durham, North Carolina. Both Amber and Paul live with an ostomy.
Q: How can people with ostomies stay healthy both physically and emotionally when facing a crisis?
Amber: The best way to take care of your emotional health is to take care of your physical health. Continue to take your supplements. Stick to a schedule and make checklists. During a difficult time, I do the same things at the same time every day and that helps. It’s also important to get enough rest and exercise, even if you have to find a routine online. Grief and anxiety can manifest physically if you don’t put those things into practice.
Paul: I agree with taking the proper supplements. Some of us with ostomies absorb vitamins differently, so it’s important to consult your doctor before starting a regimen. Exercise is also very important. As a senior in college, I was doing research with a doctor at Mayo Clinic. One day he said, “Paul, you’re getting soft and look a little out of shape – do you want to keep getting sick? You should start running and taking better care of yourself.” I had never had anyone say that before and was motivated (and a little miffed) so I started running and ran almost every day for a year. And when that same doctor performed my tenth surgery to remove my failed ileal pouch, it took only four hours instead of eight. Afterwards he said, “Your abdomen looked like you never had surgery – your adhesions were gone! Whatever you did in the last year, you should definitely keep it up!” I haven’t stopped running and exercising since.
Q: What can we do to stay healthy if we have to travel during a health crisis?
Amber: It’s important to keep a change of ostomy supplies on your person when traveling and make sure to stay hydrated. We all have leak stories. One time I was hiking in the Great Smoky Mountains and my pouch fell off. I had to change it in a porta potty! And, of course, I use hand sanitizer constantly, especially on my phone.
Paul: I’ve had leaks on planes and have had to run to the washroom with it pouring down my leg. Never a dull moment with an ostomy some days! I keep supplies in a small kit. I also always wear an ostomy belt, which helps keep my pouch secure. When my wife and I travel now we wear masks and bleach wipe everything we have to touch.
Q: Where should people turn when having a really bad day?
Amber: Stay connected with nature and focus on things that are beautiful. Take a moment and be still. Keep grounded and turn to your faith. It’s OK to cry and let those emotions out. Recognize it, feel it, and embrace it. There’s a myth that if you ignore depression it will go away. You have to deal with it before you can move ahead. Last year after my wedding I was feeling down and didn’t know why. I was too ashamed to tell anyone. So I decided to speak to my doctor. He ran some tests and it turned out that my vitamin levels were out of whack. Never be ashamed to talk to your doctor, that’s what they’re trained in.
Paul: Well, as I shared before, exercise has been a true lifesaver for me. When I’m down I also often turn to my family. Being vulnerable is hard especially when you’re sick. I often have trouble loving myself with a body that could turn on me and threaten my life at any moment. Just a few years ago, I was sick again and needed three surgeries and a prolonged hospital stay (almost a month). My wife slept every night at my bedside in the hospital. Through that I realized that perhaps I am loveable no matter what. When feeling depressed, another resource I often use is to connect to the ostomy community on Instagram and other social media. I’ve seen so many people get support from others all over the world. It’s definitely healing to share your story…and to hear others and know you are not alone.
Q: A crisis can present problems with participating in milestone events, such as graduations and funerals. How can people still stay connected?
Amber: If it’s a death, you can honor them by the way you live your life and stay positive. That’s how you can keep their memory alive. If it’s a graduation or birthday, plan something with the person or people when you’re feeling better or the crisis is over. Connection is so important. Check-in with people, even your happy friends. You never know what they’re going through. Gratefulness works too, I write down one thing I’m grateful for each day and put it in a jar.
Paul: I agree about gratefulness. In our family, we play a game every night called “3 GOOD THINGS” where we all go around and name three good things that happened each day. At our hospital, we are spending conscious time thanking people for the little things they do. Getting out of your head and thanking someone else is so essential and therapeutic. It’s so important especially if you’re down. Gratitude is as rewarding to yourself as it is to the one you’re thanking.
This is an excerpt from “Tips for Coping in a Crisis” in the Hollister Incorporated Ostomy Learning Center. Read the full article here.
Editor’s note: This article is from one of our digital sponsors, Hollister Incorporated. Sponsor support along with donations from readers like you help to maintain our website and the free trusted resources of UOAA, a 501(c)(3) nonprofit organization.
Why they Happen and What to do
Elaine O’Rourke and Ostomy Nurse and Phoenix Magazine columnist Anita Prinz discuss ostomy leaks, reasons why they happen, what to do and how to help with skin breakdown. There is lots of valuable information in this interview for even those who have had their ostomies for many years. Elaine has had her ileostomy since 2005 due to Crohn’s disease and has had her fair share of leaks over the years until finding the right pouching system for her. If you are having persistent leaks then you should always consult with an ostomy nurse who can help find a solution for you.
You can find Elaine on Facebook and her “3 simple ways to overcome fears about your Ostomy” program at www.ElaineOrourke.com/ostomyprograms/
Tag Archive for: leaks
Nothing Found
Sorry, no posts matched your criteria
Contact Us

United Ostomy Associations of America
P.O. Box 2293
Biddeford, ME 04005-2293
Call us toll-free at: 1-800-826-0826.
Our Information Line hours are Monday-Friday, 9am to 3pm EST. If you have an emergency, please dial 911 or contact your local medical professional.
Please understand that UOAA is a private, nonprofit, advocacy and informational organization. We are not a medical facility and we do not have medical or legal professionals on staff. Therefore, UOAA does not provide Medical, Mental Health, Insurance or Legal Advice. Visit UOAA Virtual Ostomy Clinic provided by The Wound Company for non-emergency, virtual ostomy support.
Get Involved
UOAA is the leading organization proactively advocating on behalf of the ostomy community. Recognizing that we are always stronger together, we encourage everyone to get involved by joining our Advocacy Network. We’ve also created several Advocacy Tools and Resources to help you successfully advocate on behalf of the ostomy community to ensure every ostomate receives quality care.

