Embracing Ostomy Advocacy and Giving Back
By Angie Davenport
I’ve had my ileostomy for 38 years due to ulcerative colitis but I only recently went public to encourage other ostomates. Over the years I’ve helped many individuals by word of mouth while keeping my ileostomy private to the outside world. I have always wanted to be a blessing on a wider scope though to others with ostomies.
I was first diagnosed with ulcerative colitis in 1980 when I was three months pregnant. At first, I thought it was pregnancy symptoms. After a major episode, I was treated with medication for ulcerative colitis. My son, James was born a few weeks early due to complications.
After the birth of my son in March of 1981, everything was under control and I eventually relocated from Warren, Ohio to Atlanta, Georgia. While living in Atlanta I had a major setback with ulcerative colitis and I had to fly back to Ohio immediately and went directly to the hospital.
After several weeks of treatments in the hospital, my doctor came into my hospital room one night and said we have to do surgery or you won’t make it 24 hours. I’ll never forget my mom crying and praying for God to give her my disease so I could have a normal life.
When I received my permanent ileostomy in March of 1982 I was a young 23-year-old single mom. It was the day before my son’s first birthday. I had never heard of an ostomy. When I woke up in ICU I was devastated, ashamed and frightened. I thought my life was over.
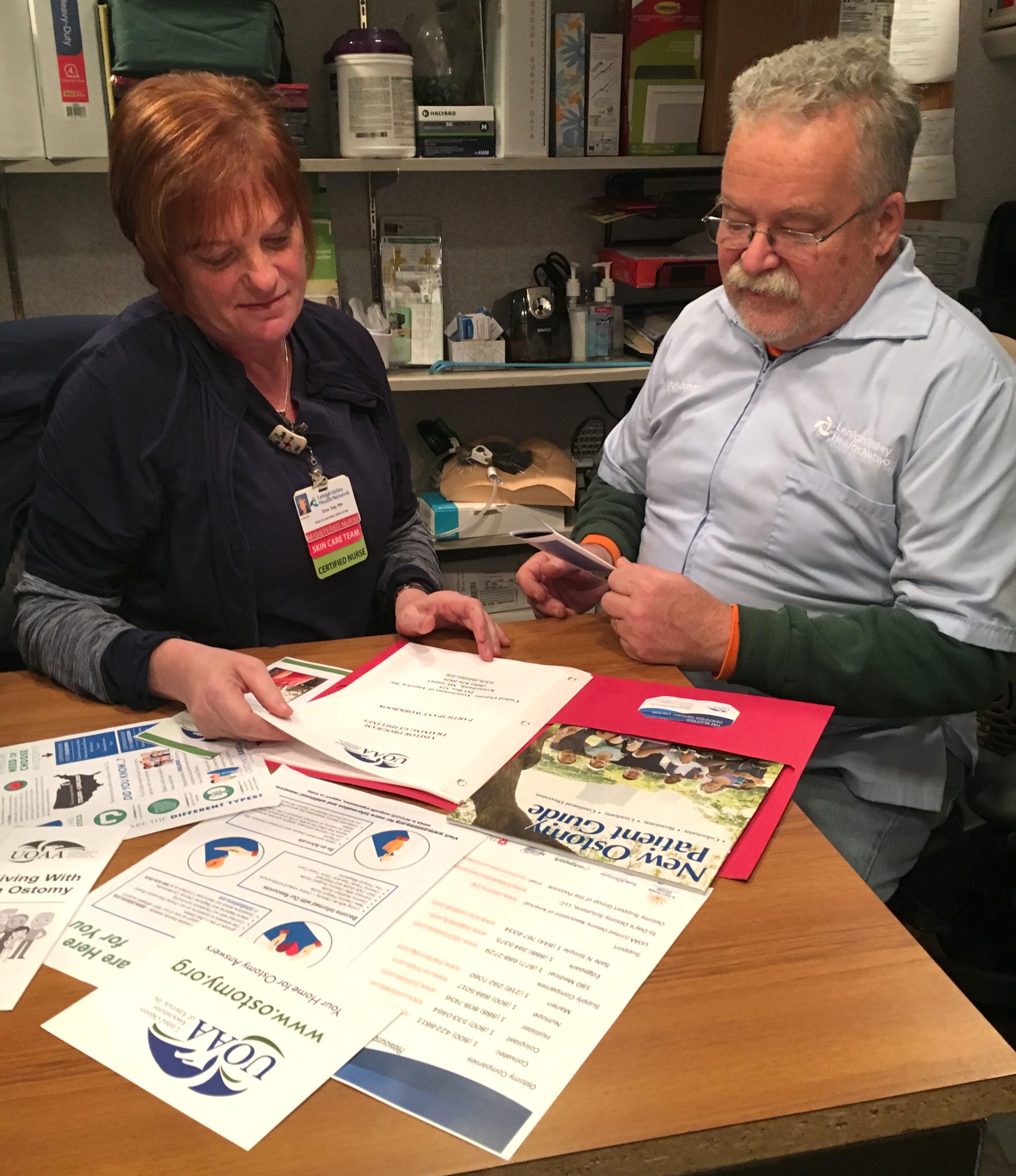
Once I became strong enough physically and mentally I moved back to Atlanta. I was still feeling ashamed and frustrated until my physician in Georgia recommended I attend the local United Ostomy Association (the precursor to UOAA) support group.
While living in Atlanta I became very involved with the UOA group and completed the visitor training program. I enjoyed visiting new ostomates at the hospital. I felt the freedom to be involved because no one really knew me in Atlanta. I remained active until I relocated back to Ohio in 1985. That same year I married my high school sweetheart and we will celebrate 36 years of marriage in November.
Although I was very private about my ostomy I was very successful in my career. I became the first African American female officer at our local bank and functioned in several positions without the exposure of my ileostomy. After the downsizing of my employer, I later worked 10 years at Great Lake Cheese until retiring in 2016.
What is my purpose in life? How can I make my mom proud?
I’ve enjoyed my life as an ostomate. I love traveling, cruising and shopping. I was known in the business community as a person that loved to dress. I taught Dress for Success at the bank for all new tellers.
 The past few years were filled with so much grief, with the most current being the death of my mom on July 4th 2019, only three days after my 60th birthday. I was feeling the deep void of losing a brother and both parents within 4 years, depression was setting in. I had support but I felt helpless and lost. What is my purpose in life? How can I make my mom proud?
The past few years were filled with so much grief, with the most current being the death of my mom on July 4th 2019, only three days after my 60th birthday. I was feeling the deep void of losing a brother and both parents within 4 years, depression was setting in. I had support but I felt helpless and lost. What is my purpose in life? How can I make my mom proud?
Most will remember 2020 as a horrific year with so much sickness, death and devastation from a deadly pandemic. For me, I utilized the time to seriously seek God for a purpose in my life and being quarantined turned out to be a blessing in helping me find my purpose.
I knew my testimony would bring awareness and hope to so many people.
I became more involved via social media with other ostomates. I’ve met some wonderful friends and it became rewarding to encourage others that had shared similar experiences as me. My heart was really saddened when I read an article about a young man that had gone to court for the right to die because he didn’t want to live with an ostomy. I wept. Also seeing how some individuals can’t afford the basic ostomy supplies and had to use grocery store bags and tape to secure their ostomy bags was heartbreaking. I knew then, that there was so much more I could do for the ostomy community. I knew my testimony would bring awareness and hope to so many people.
As a member of Jearlean Taylor’s Ostomy Stylzz Facebook Group I participated in a virtual fashion show. She is a personal inspiration to me and that show boosted my confidence to a much greater level. I felt a relief to go public. I chose August 14th, 2020 to go live on Facebook and share my story. I felt such freedom once I finished. There were family members, coworkers, church and community friends that responded and supported me in disbelief. For the past 38 years, they never knew I had an ostomy.
One family friend messaged me and told me that he was scheduled for surgery but has canceled many times, but because of my video he felt he could now go through it. I still check on him to make sure he’s not having any problems. That made going public all worth it. But what else could I do?
I decided to participate in the Run for Resilience Ostomy 5K. I registered over 20 walkers to participate virtually in several cities and I exceeded my fundraising goal by almost 100%. The highlight of the day was my local mayor stopping by to present me with a proclamation from the City of Warren in support of ostomy awareness. Our local newspaper also highlighted the event.
…because of my video he felt he could now go through it.
After posting my Ostomy Awareness Day photos and story on Facebook I was contacted by so many family and friends willing to support me in the future.
With the pandemic still active, I’ve been limited in getting out in the public but I do try to make an effort to encourage other ostomates daily. I’ve connected with my local Affiliated Support Group leader and I’m looking forward to greater things once we can meet publicly.
On, March 6, 2021 I will be a 39-year ostomate.
I’m on Facebook and I have a Youtube video discussing my ostomy journey.
I’m free, living with my ostomy!

 My journey with Short Bowel Syndrome (SBS) spans 61 years, and it has been full of twists and turns. I’ve often wished that I understood from the beginning exactly what it meant to have SBS – it is not temporary, rather it is chronic. That means it’s a lifelong condition, and it has frequently caused me to make adjustments to maintain my independence and lead a productive and meaningful life. Reaching independence and self-reliance took years of learning the importance of self-advocacy to get the information I needed from my healthcare providers, no matter how difficult it may have been to hear that information. Each symptom, diagnosis, ostomy and medical procedure that preceded my eventual SBS diagnosis posed new challenges. The more I knew about what lay ahead for me, the more I could take charge of my own life. As August marks SBS Awareness Month, I hope my experiences will help inform and inspire others living with this serious and chronic malabsorption disorder to speak up and ask for information and tips to help maintain as much independence as possible.
My journey with Short Bowel Syndrome (SBS) spans 61 years, and it has been full of twists and turns. I’ve often wished that I understood from the beginning exactly what it meant to have SBS – it is not temporary, rather it is chronic. That means it’s a lifelong condition, and it has frequently caused me to make adjustments to maintain my independence and lead a productive and meaningful life. Reaching independence and self-reliance took years of learning the importance of self-advocacy to get the information I needed from my healthcare providers, no matter how difficult it may have been to hear that information. Each symptom, diagnosis, ostomy and medical procedure that preceded my eventual SBS diagnosis posed new challenges. The more I knew about what lay ahead for me, the more I could take charge of my own life. As August marks SBS Awareness Month, I hope my experiences will help inform and inspire others living with this serious and chronic malabsorption disorder to speak up and ask for information and tips to help maintain as much independence as possible. Six years later, I found myself unable to eat due to severe abdominal pains and a pseudo-obstruction and was put back on TPN. I feared this would prevent me from traveling on a three-week family trip to Australia, but my husband and daughters learned how to properly store, prepare and administer my TPN infusions, so we could still travel. I am so grateful to have been able to enjoy that trip with my family despite my TPN, ostomy and needing to use a catheter.
Six years later, I found myself unable to eat due to severe abdominal pains and a pseudo-obstruction and was put back on TPN. I feared this would prevent me from traveling on a three-week family trip to Australia, but my husband and daughters learned how to properly store, prepare and administer my TPN infusions, so we could still travel. I am so grateful to have been able to enjoy that trip with my family despite my TPN, ostomy and needing to use a catheter.