Ostomates Provide Insight to Lawmakers on Behalf of UOAA
By Ellyn Mantell and Michael Quear

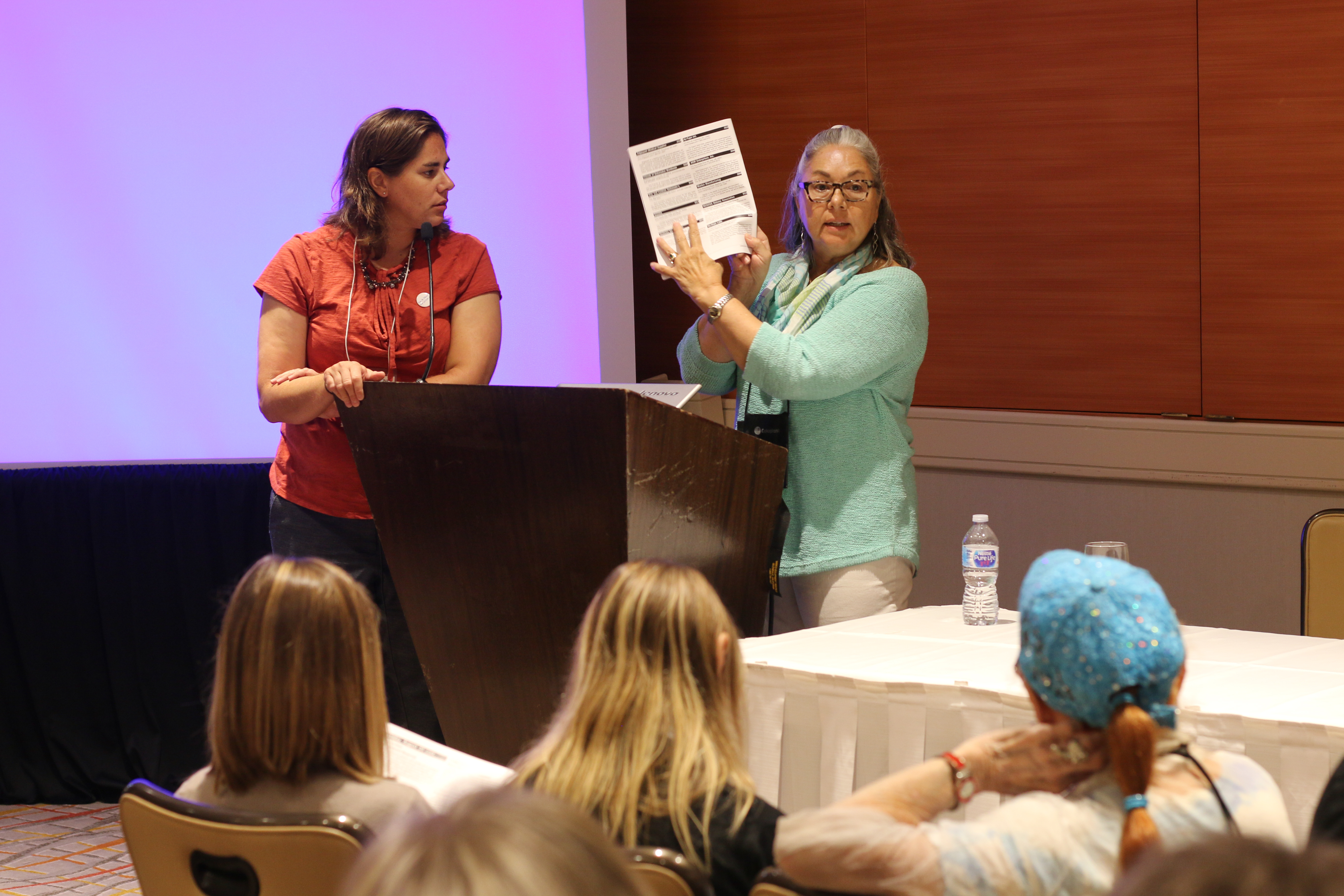
Left, Ellyn Mantell with UOAA Advocacy Manager Jeanine Gleba, right, outside New Jersey Senator Cory Booker’s office.
UOAA Representative – Ellyn Mantell
There is so much frustration and dissatisfaction around the government right now, that it is easy to forget all of the wonderful things that continue to be done behind the scenes, and I want to share with you my experience in that regard. On Sunday, March 3, 2019, my wonderful support guy, husband, Bruce, and I traveled to Washington, DC to attend the annual Digestive Disease National Coalition meeting. I was asked to be a Patient Advocate accompanying Jeanine Gleba, Advocacy Manager for United Ostomy Associations of America. She and I have a special bond, since she lives in New Jersey and has attended support groups’ meetings with me, and we both have the same goal, which is increasing awareness and getting the most for ostomates.
After meeting key personnel and greeting other attendees on Sunday night, I felt empowered to be part of Team 5 the next day, when we would go to “the Hill!” Monday morning, following a warming breakfast (which we needed since it was windy and oh, so cold walking up toward the Capitol) and a basic logistics session, we headed to the Hart Building, not actually on “the Hill” but very exciting, nonetheless. I saw the offices of Senators about whom I had read or seen on television…a rare opportunity to be in the “Place Where It Happens”!
Our team was awesome and so inspiring! In addition to Jeanine and my presentation (visual aids are great, and my emergency kit pouch was a surefire way for the Legislative Aides to get the point: the necessity for funding for supplies, etc. as well as not being denied benefits for pre-existing conditions) we had two other Patient Advocates. Carolyn was invited by Megan Glynn, Manager of National Programs for the American Liver Foundation, and she is alive because of a living donor liver transplant. This is quite amazing, since the liver is composed of two lobes. One lobe can be transplanted and both donor and donor recipient’s livers will regenerate. It is truly amazing! Carolyn was making a request her life-saving medications, which cost thousands monthly, may bankrupt a family trying to keep alive the patient they love…a terrible choice to have to make. Generics and off label usage may make a huge difference, but funding is always the issue.
Cheryl Velba then spoke with the Legislative Aides about her Short Bowel Syndrome, she is a Rare Disease Advocate. Surviving the removal of most of her colon and small intestine, she is one of the few to survive such a severe twisting of her bowel. This life-threatening occurrence, and the damage done to her body includes not only digestive issues but ocular ones, as well. She is asking for certain medications, again, costing thousands a month, be switched for generics or off-label usage. We all urged the aides to impress upon the Senators for whom they worked to limit out-of-pocket costs as well as curb current and future payer tactics to shift costs onto the patient.
The Digestive Disease National Coalition stands for Research of Digestive Diseases; Patient Access to Affordable, Quality Health Care; and Prevention and Awareness of Digestive Diseases. Digestive Diseases are chronic and, in many cases, debilitating and disabling. I was deeply honored to be able to bring awareness to the young aides who may not have known anything about our issues before yesterday, but when we were done, had to have learned another slice of life, the struggles of many…and hopefully, they will impress that upon our NJ legislators, Senator Menendez and Senator Booker.
UOAA Representative – Michael Quear
I recently attended the Digestive Disease National Coalition Annual Spring Public Policy Forum as a representative for UOAA. Actually, I participated in a group that was meeting with Congressional staff. My group was made up of Pennsylvania residents; so we met with staff of the PA Senate delegations and selected House Members staff. In my group I was the only person with an ostomy, but I certainly had experience with a digestive disease!
I was diagnosed with ulcerative colitis when I was 14; 4 years later I had my surgery – a total colectomy with a permanent ileostomy when I was 18. It’s hard to believe that was 42 years ago. Plus, I certainly knew my audience. I’d had the privilege of serving as professional staff for 20 years on the Committee on Science Space and Technology in the US House of Representatives.
I know these are busy folks and that we would likely have only 20, at best 30 minutes of their time. (We actually only had 15 minutes!) So I thought what are the points I would like them to remember about life for an ostomate and what impacts what they do by allocating funding and how healthcare policy impacts people like us.
First off, show and tell. When you say the word colostomy most people think a bag filled with et cetera. An ileostomy draws a blank stare. So I took along the appliance I wear, so they could feel it, see exactly what it looks like and how it works. Using my thumb I explained my stoma. I also explained that despite the revolutionary advances in medical diagnostic equipment, prosthetics and drugs that in ostomy products there have not been many major breakthroughs in ostomy solutions, but research funding targeted for ostomy products could change this.
I also talked about the stigma that ostomates often feel. In general, an ostomy is something some in the public feel is only slightly worse than death. I was 19 when I heard someone say, “I’d rather be dead than wear a bag….” And I’ve heard similar remarks occasionally thru the years. As it is national Colorectal Cancer Awareness Month, I mentioned that people who suspected they had a serious gut issue were afraid to be seen by a doctor because of this stigma. I recommended their boss use his public platform to remind people this is a procedure that saves lives, not ruins them.
Finally, the cost. I told them the cost of my appliance and that some people need to change it daily, others every 4-5 days. Regardless, over the course of a year costs add up. Therefore, it is important that insurance and government programs cover these costs. When Congress fiddles with health care funding and/or policy they need to think about people like me with serious gut disease in general.
Was it a long day? Yes! Was it useful – I hope so!
But I think it is one that the staff will remember.


 Wow. Right?
Wow. Right?



 The model, Gaylyn Henderson, has been sharing her infectious positivity with the ostomy community for years including in a past
The model, Gaylyn Henderson, has been sharing her infectious positivity with the ostomy community for years including in a past 

