2019 Advocacy Accomplishments We Can All be Proud of
By UOAA Advocacy Manager Jeanine Gleba
I pride myself on being an “action person” and nothing gives me greater satisfaction than checking those boxes and crossing off items on my lists to-do (daily, short-term, long-term etc) both in my personal life and professionally. So I get super excited at year-end when I can reflect and look back at all that UOAA has accomplished in our advocacy efforts! I’m happy to report 2019 was not an exception. Although many priorities are ongoing and I can’t actually cross them off my list, I remind myself that Rome was not built in a day and realize to make a major impact in the health care world it could take many years. The important thing for all of us to remember is that we are making progress and positive change is happening.

Ostomy advocates at the DDNC Public Policy Forum in March.
Each year UOAA’s Advocacy Committee establishes annual goals based on the strategies outlined in UOAA’s Advocacy Agenda. We have learned that the needs of the ostomy community are fluid and more often than not, I find each year that new priorities must get added to the list. These goals and priorities keep us organized and ensure we stay focused on where we can have the most effect given our organization’s limited resources.
In no particular order and not an all-inclusive list below will give you an idea of what we worked on and accomplished in 2019. This does not include Ostomy Awareness Day efforts as they were previously shared:
Completed the “Expect More: Take Control of Your Healthcare” self-advocacy toolkit with checklists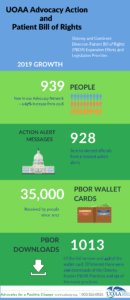 – All of the parts and resources are online here. In 2019 there were 579 downloads of the resources and the ostomy supply checklist had the most downloads at 247.
– All of the parts and resources are online here. In 2019 there were 579 downloads of the resources and the ostomy supply checklist had the most downloads at 247.
Best in Practice Research Project Launched – The purpose of this research project is to examine components of UOAA’s Ostomy and Continent Diversion Patient Bill of Rights (PBOR) and demonstrate best in practice standard guidelines for ostomy care. In 2019 we collected the data, in 2020 we will conduct the data analysis phase, publish results and ideally find ways to use the results to improve patient outcomes.
Centers for Medicare and Medicaid Services (CMS) Ostomy Supply Policy
- Conducted an online survey earlier and analyzed results to better understand the issue of obtaining greater than allowable quantities for those that have a medical necessity such as a high output stoma
- Submitted comments and recommendations from UOAA to CMS for the Simplifying Documentation Initiative (SDI) and the Patients Over Paperwork Initiative to reduce burden as it relates to the ostomy supply process.
- We have a subcommittee comprised of medical professionals, manufacturer representatives, and patient advocates who will continue this effort in 2020.
Legislative Priorities
- Advocated on the Disability Integration Act (DIA), Removing Colorectal Screening Barriers, Ostomy Awareness Day, Step Therapy, and Competitive Bidding Program
- Released two new position statements for DIA and Opioids
- Supported the DDNC Step Therapy National Day of Advocacy
Additional Efforts to Expand Patient Bill of Rights 
- Safe n Simple is now including the PBOR Wallet Card in new ostomy patient starter kits and Byram Healthcare now includes it in their ostomy educational booklet
Further Advocacy Outreach and Collaborations
- Upfront with Ostomies Column: As a result of contacting the editor of the Wound Management Prevention journal UOAA now has its own column in this clinician journal. 5 articles were published in 2019
- UOAA was invited by the CMS Quality organization to submit a new idea for the 2021 Improvement Activities used in the Merit-based Incentive Payment System. Ex-committee Member Barbara Dale and I submitted for consideration two modifications to existing improvement activities that focuses on re-evaluation of ostomy care and supplies
- Access and Care Coalition: Successfully continued to ensure Congress refrains from expanding the Medicare Competitive Bidding program to include ostomy and urological supplies
- 3172 people downloaded the TSA Travel Communication Card
- Started efforts with OEM of LAX airport in CA to make restroom improvements for ostomy accessibility; created UOAA guidelines for United States ostomy restroom accommodations
- Between myself and members of the Advocacy Committee we authored or contributed to 18 magazine and UOAA e-newsletter articles on advocacy-related topics
Looking forward to greater achievements in 2020!


