By Steven Berit
I fainted the first time I lost a tooth. Not from the actual pain of the removal, but from the sight of the blood dripping from my mouth. I also fainted during a health talk in the sixth grade. Most people would call me “squeamish,” and I would agree. The sight of blood or even the mention of anything related to the human body can easily send me into a spiral of emotions typically resulting in me waking up in the nurse’s office. So, you can imagine my apprehension when the doctors first suggested the idea of me receiving a colectomy.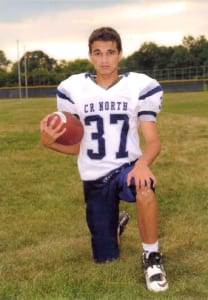
Hi, I’m Steven Berit. I’m eighteen years old and I am a senior in high school. I live in Pennsylvania with my mom, my dad, and my sister when she is home from college. I live a pretty “normal” life. I go to school, play football, and hang out with friends just like anyone else my age would do. The only difference between me and everyone else is that I have an ostomy bag and they don’t. This small detail isn’t even noticeable for most, but at first, it certainly was noticeable to me.
I was sixteen when I was first diagnosed with ulcerative colitis. The next year and a half would be full of trial and error, and with each passing day the errors stuck out more and more. Mesalamine, Remicade, Entyvio, and Xeljanz were just a few of the never-ending drugs that I was prescribed. The only thing that seemed to be working was steroids, but both my doctors and my acne-ridden face agreed that this was not a permanent solution. Finally, in July of 2019 while in my latest stint on the 5th floor of the Children’s Hospital of Philadelphia, I made the decision to say good-bye to my very inflamed, friend- my colon.
I don’t remember much of the first night following the surgery, but the next couple of days stick out in my mind vividly. Well, I mean I clearly remember the restless nights. As for the actual stoma itself, this took me some time before I had my first encounter with it eye-to-eye or eye-to-intestine in this case. The second night was one of the worst nights of my life. I guess the anesthesia had worn off and with it came the regret. Yes, that second night I thought I made the biggest mistake of my life. There I laid in a hospital bed way too small for my eighteen-year-old frame contemplating if I could ever recover from this setback in my life.
Well, the sun rose and with it time for my first bag change. I remember screaming- a lot. They told me that the stoma couldn’t feel pain, but what they failed to mention was that I could still feel the pain of my hair ripping off my body as they pulled the adhesive off my skin. Trust me your average eighteen-year-old boy has plenty of hair to go around, but your eighteen-year-old boy that has been steroids for the last year and change has more hair than one would openly like to admit. But, as the bag came off, I got my first glimpse of my future in the form of a beautiful, red stump known as my stoma.
The next couple of weeks would come and go with relatively little struggle, but as summer came to an end my biggest challenge approached- going to school. I tried every possible combination of tucking my bag into my pants until I came to the realization that no one cared. Either people didn’t take notice of the bag of stool attached to my body or they too were busy and caught up with their own lives to care about what secret I kept hidden behind my shirt. It was my first time since being diagnosed with UC where I felt “normal” at school. Which was odd because to most this was the least “normal” I had ever been.
No, my journey with my ostomy was not one I would describe as love at first sight. But it has grown on me over time. Yes, I still need my parents help to change my bag every three days, but the once shrieks of pain have now subsided into murmurs. I now go to school every day like a new person. I no longer have fears of finding where the nearest bathroom is or if I am going to be able to take a test for thirty minutes without a wave of urgency coming over me forcing me to drop everything and make a mad dash to the nearest restroom. Instead, most days go by without any thoughts of UC or stomas crossing my mind.
As I come closer every day to my reversal surgery in December, I begin to wonder if I would be able to live with this bag for the rest of my life, and after some thought, I honestly believe I would be able to. UC has taught me over the years that I can overcome anything and the ostomy bag was just the latest thing I had to overcome. If I can go from fainting over a loose tooth to conquering a disease that once bullied me then I can overcome any challenges that may come my way. The once terrifying ostomy bag has become a cherished friend of mine who I will never forget even when it is gone. I cried when I had my first tooth removed. I may also cry when I have my ostomy removed, but I think these tears will fall for a completely different reason.


 Living 10 steps from death’s door can take an emotional toll. My name is Makeda Armorer-Wade and I am an inspirational life coach and bes
Living 10 steps from death’s door can take an emotional toll. My name is Makeda Armorer-Wade and I am an inspirational life coach and bes Sometimes listening to the despair of my fellow ostomates and experiencing my own despair at times, for lack of knowledge is what spurred me into action. I wanted to be an example, that there is still life to be lived after an ostomy. Our mindset is important. Where our mind goes, the body follows. Life is what we make of it.
Sometimes listening to the despair of my fellow ostomates and experiencing my own despair at times, for lack of knowledge is what spurred me into action. I wanted to be an example, that there is still life to be lived after an ostomy. Our mindset is important. Where our mind goes, the body follows. Life is what we make of it. So, I share with others that having an ostomy is just an alternative way of going to the bathroom. We all have to go the bathroom. But now, I have the benefit of having more control over when I go. An ostomy is life-saving. An ostomy is an opportunity to really live your best life on purpose.
So, I share with others that having an ostomy is just an alternative way of going to the bathroom. We all have to go the bathroom. But now, I have the benefit of having more control over when I go. An ostomy is life-saving. An ostomy is an opportunity to really live your best life on purpose.



 After eight years of not responding to western pharmaceuticals, at the age of thirty, I found myself facing a colectomy. While I had anxiety about the ostomy surgery and fear of the unknown, my overall emotion was relief. This surgery was hopefully going to be the end of many years of pain and suffering. Thanks to the encouraging words of other ostomates I was wheeled into surgery with a smile on my face, excited about what the future would hold for me–I saw endless possibility!
After eight years of not responding to western pharmaceuticals, at the age of thirty, I found myself facing a colectomy. While I had anxiety about the ostomy surgery and fear of the unknown, my overall emotion was relief. This surgery was hopefully going to be the end of many years of pain and suffering. Thanks to the encouraging words of other ostomates I was wheeled into surgery with a smile on my face, excited about what the future would hold for me–I saw endless possibility!

