By Cheryl Ory, UOAA President
President Biden has proclaimed March 2023 National Colorectal Cancer Awareness Month. The American Cancer Society says that colorectal cancer is the third leading cause of cancer related deaths in both men and women. On another note, the death rate has been dropping for several decades. One reason is that treatments have improved. Another reason is that colorectal polyps are now being found more after screening and removed before they can turn into a cancer.

UOAA Advocate, ostomate and colorectal cancer survivor Allison Rosen speaks on the National Mall as part of the United in Blue Rally sponsored by Fight Colorectal Cancer. Video: United in Blue Rally on the Mall (1)
In 2008 I was diagnosed with Stage 3b colorectal cancer. I was told the cancer had been developing for at least 10 years or more, most likely when I was in my early 30’s. There was a polyp, if it had been removed at an earlier date the cancer would not have developed. After radiation, chemo, surgery, and more chemo I am now a colorectal cancer survivor with a permanent colostomy, an ostomy that has saved mine and others lives from not only cancer, but other debilitating diseases.
I’m happy that UOAA is standing alongside partner organizations like Fight Colorectal Cancer to push lawmakers into giving attention to the alarming rise in young people with colorectal cancer.
With younger people being as risk and diagnosed , The U.S Preventative Services Task Force lowered the recommended screening age to 45 in 2021. One in five colorectal cancer patients is between the ages of 20-54. Talk to your doctor about options for colorectal cancer screening. As the Colon Cancer Coalition states with earlier screening and detection, “Colorectal Cancer can be Preventable, Treatable, Beatable.”
If you are a person still at risk, like those with IBD, let me urge you to get screened. Screening can result in any colorectal cancers being found earlier when they are easier to treat.
Here at United Ostomy Associations of America (UOAA) we have a long legacy of supporting the survivors of cancer and many other conditions so that they can have best quality of life possible. If your cancer requires a life-saving ostomy surgery remember-you are not alone. 725,000- 1 million people in the U.S. of all ages and backgrounds live with an ostomy.
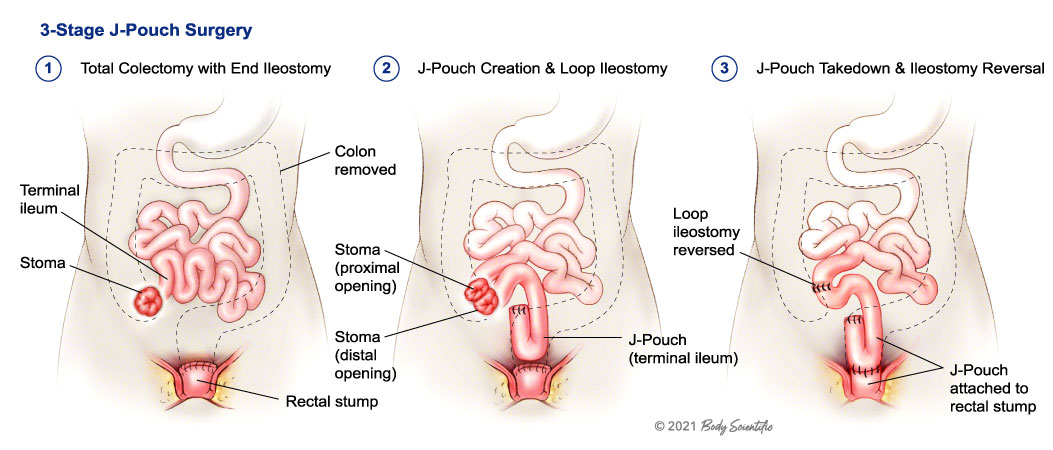
 Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary ileostomy (from the small intestine) or colostomy (large intestine). This may be required to give a portion of the bowel a chance to rest and heal. When healing has occurred, the colostomy can often be reversed and normal bowel function restored. It’s important to know that not everyone with an ostomy will be a candidate for a reversal operation. A permanent colostomy may be required when a disease affects the end part of the colon or rectum.
Every individual person’s disease treatment is unique but ostomy surgery for colorectal cancer may mean a temporary ileostomy (from the small intestine) or colostomy (large intestine). This may be required to give a portion of the bowel a chance to rest and heal. When healing has occurred, the colostomy can often be reversed and normal bowel function restored. It’s important to know that not everyone with an ostomy will be a candidate for a reversal operation. A permanent colostomy may be required when a disease affects the end part of the colon or rectum.
We have new Living with a Colostomy guide and ileostomy guide to help you learn as much as possible before or after you have this life changing surgery.
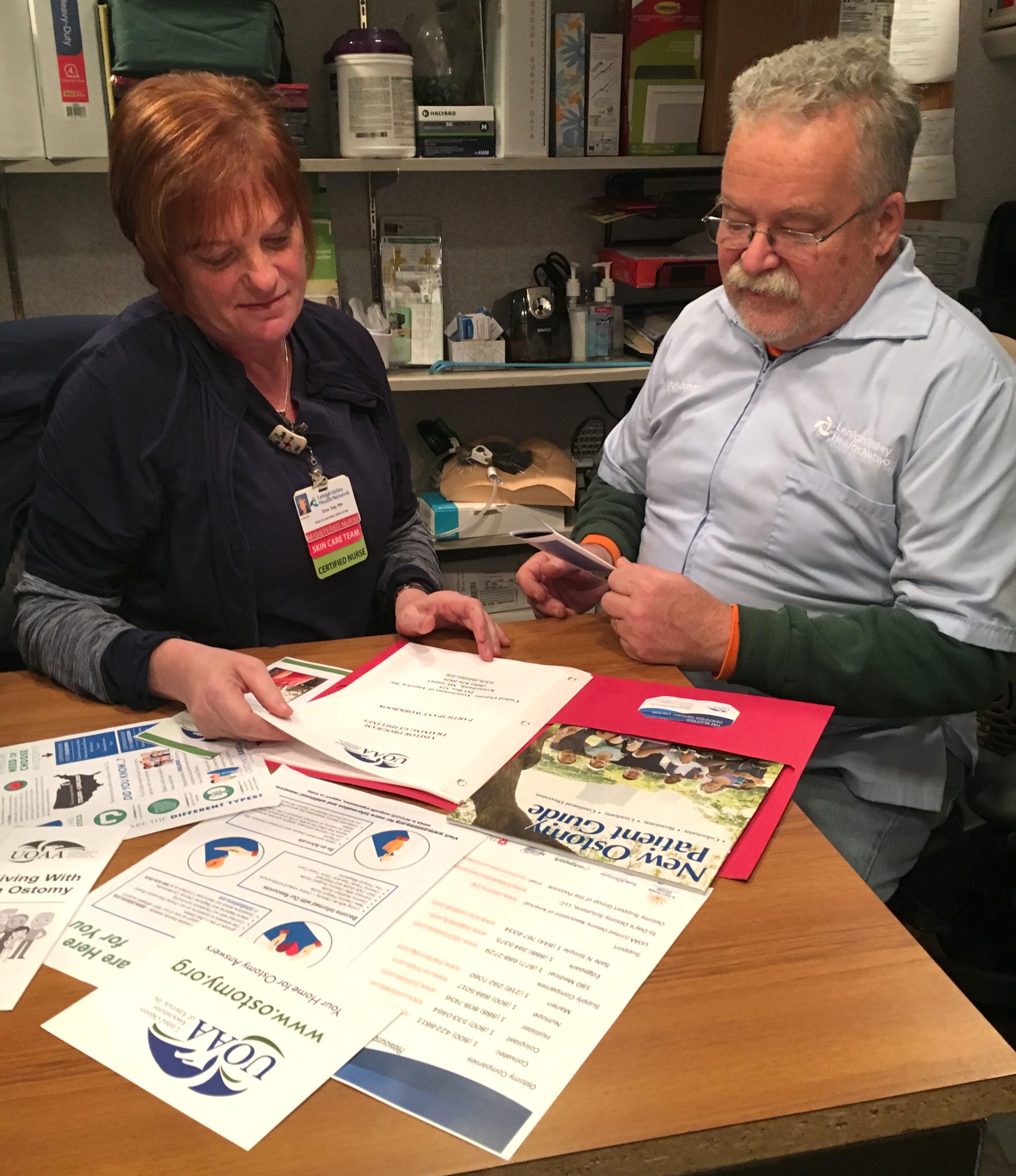
It’s especially important to connect with one of hundreds of UOAA Affiliated Ostomy Support Groups in the U.S. before, or shortly after, your surgery. Peer support and preparation can put you on the path to success in what may be a challenging time both emotionally and physically. Ask if the hospital has a certified ostomy nurse and insist on having your stoma placement marked before surgery. These and other self-advocacy tools are paramount and outlined in our Ostomy Patient Bill of Rights.
You may feel too overwhelmed as you are discharged at the hospital to fully understand ostomy pouching systems and accessories and lifestyle considerations. If you have a medical question contact your doctor or nurse, but if you have a quality of life question-UOAA resources here at ostomy.org and peers at UOAA Affiliated Support Groups likely have the answers.
It’s important to learn the facts about living with an ostomy. After the healing period outlined by your surgeon you can swim, bathe, be intimate, travel, and embrace a new normal life. After some trial and error, you may also eat most of the foods you have been able to eat in the past. Education is key to battling misinformation.
Unfortunately misinformation and stigmas surrounding both ostomy surgery and colorectal cancer affect the number of people getting screened or getting the medical treatment they need. Let’s work together to educate, advocate and support survivors.
Cheryl Ory is a colorectal cancer survivor who received a permanent colostomy in 2008. Cheryl is a Registered Nurse who has had a passion for volunteering with the ostomy community ever since and first joined UOAA’s Board of Directors in 2015. She now holds the position of President.

 another proud scar.
another proud scar.