Expect More – Take Control of Your Health Care
Part 4 in Series
By Susan Mueller, BSN, RN, CWOCN and UOAA Advocacy Committee
“Details matter. It’s worth getting it right.” ~ Steve Jobs
The Buck Stops Here
Since UOAA started the advocacy campaign we have been stressing that YOU are your own best advocate. This may be hard to believe since the whole business of insurance is so overwhelming that it feels like a David and Goliath story. Like anything else, once you understand the rules of the game it makes it a lot easier. You actually have a bigger part in the game then you may know. Often consumers of medical care, patients, people like you, think that everyone knows their story. You are asked a million questions every time you pass through the doorway of any hospital or doctor’s office and everyone is writing things down. How many times do you have to tell your story? Answer: as many times as it takes to get the results you want. Unfortunately, the goal of great communication among the players in the healthcare game has not been reached, and all these computers do not talk to each other as much as you think. So what this means is that you have to make sure that everyone knows the important parts of your story and that they understand what you need.
So it goes like this, the people who pay the bills want to make sure that the money that is paid is according to their rules; that is, for a medical reason. So the people who are asking to be paid have to explain that the service or supply is medically necessary. For example, the company that sends out your supplies (ostomy supply distributor) has to be able to say that you need the supplies because you have an ostomy, what kind of ostomy you have, why you have an ostomy, and when you had your surgery. Then if you have Medicare they have to ask you questions to make sure someone else is not giving you supplies (like a home care agency or nursing home or hospital) because Medicare doesn’t want to pay double. The doctor or physician’s assistant or nurse practitioner has to report some of the same things plus show in their notes (your medical record) they have spoken to you about your ostomy and what you need for your care. This is where you come in; you have to make sure your doctor knows what you need and why, even though your doctor may know very little about ostomies.
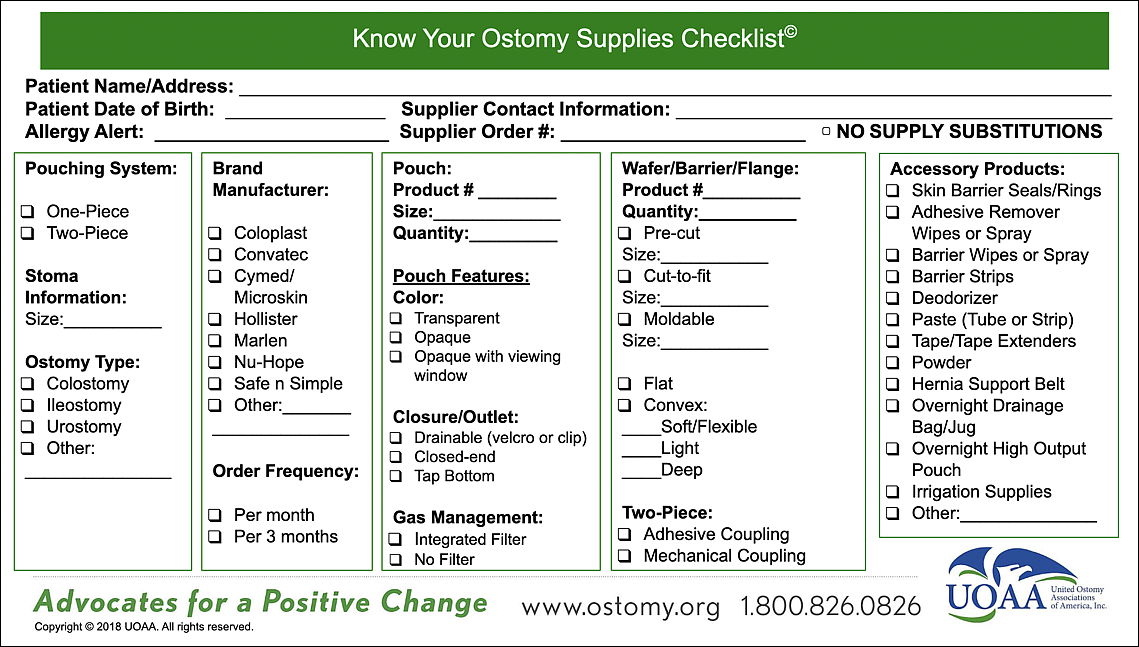
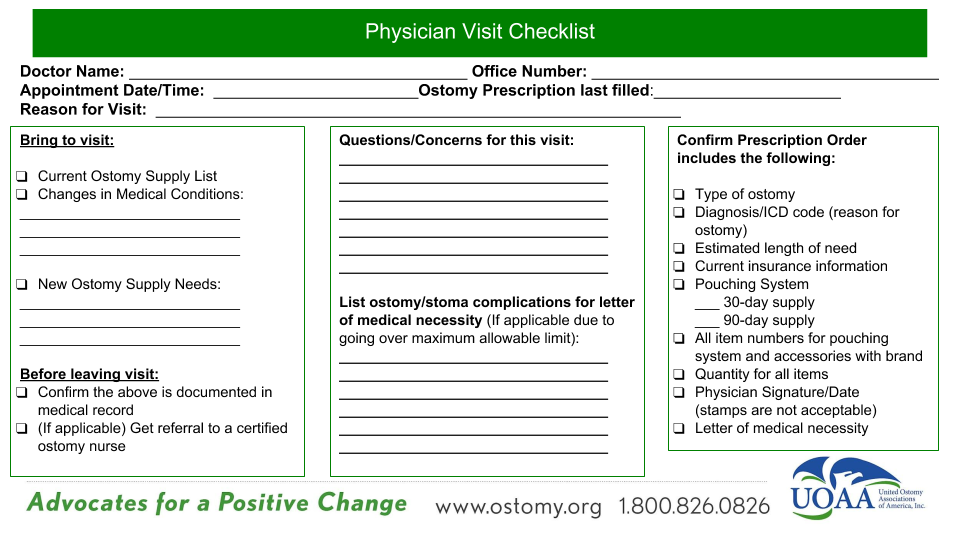
Get More Involved with your Doctor in Your Healthcare
A good suggestion is to visit your healthcare provider (doctor, nurse practitioner, physician assistant) at least once a year and provide a supply checklist which includes all the supplies you need (with the product numbers), and what type of ostomy you have. At this visit discuss what has happened in the last year; for example, you had a yeast infection around your stoma, you went to the emergency room for an obstruction or dehydration, you developed a hernia around your stoma, you gained or lost weight and had to change your type of ostomy product… This is the kind of information that needs to be in your medical record. Your medical care provider may then give you a referral to an ostomy nurse at a wound or ostomy clinic, or a dermatologist or may just write it down in your record so when the insurance company wants to know why you now need a belt or a different kind of pouch or a greater quantity of pouches, they will know why.
Medicare has done research to figure out how many supplies an “average” person with an ostomy usually needs. If what you need is different, then your doctor must include information on your medical condition to support the need for the type and quantity of items ordered. If you are working with a nurse who is specially educated about ostomies, the nurse may also be able to help you by writing down why you need different supplies than the average ostomate and give that information to your doctor to put in your medical record. This information in your medical record can then be given to your ostomy supply company and or your insurance. It is then the responsibility, under Medicare guidelines, of your supply company to get this information from your medical provider.
An example of a special situation that would require additional supplies might be that your skin is irritated from frequent leakage of your pouching system due to your stoma being flush to the skin or below the skin. You require frequent pouch changes until your skin can heal. Any request for supplies more than the average amount is marked for review. Just because a person “wants” more is not a good enough reason and those requests for supplies (claims) will be denied. You might have to have detailed notes in your medical record about why you need to use a convex wafer or pouch (such as because you have a stoma which is below skin level, or the stoma opening is at skin level).
Medicare has specific guidelines for the coverage of ostomy supplies, including that they be used exclusively for colostomy, ileostomy or urostomy management. Ostomy pouches being used to manage fistula or wounds are not covered under Medicare guidelines.
Be aware that suppliers will not receive payment from Medicare for the items that are ordered if your physician did not provide the proper detailed information from your medical records when it is requested or if your detailed written order (prescription) is missing information like a signature. Furthermore, not providing this information may result in you, the patient, having to pay for the item yourself. Note that your doctor’s cooperation is a legal requirement as outlined in the Social Security Act, the law governing Medicare.
To help you better prepare for your next office visit, please use this new checklist resource.
Pay Attention to the Details
The details are important, sometimes a date is wrong, the type of ostomy is wrong, the code for your diagnosis has a number missing…your insurance was not recorded or was recorded incorrectly, the doctor didn’t sign the note. Those things are minor and require a little detective work. So if you have a request (claim) denied you may have to be a detective. You can speak with someone at the company who provides your supplies (ostomy supply distributor) and ask them to help you understand why your request (claim) was denied. Maybe together you can discover that a number was off or incomplete information was submitted. Another example of an ostomate taking control of their healthcare is to not assume that your supplier has the proper documentation, but to ensure that your file at your supplier does include all of the necessary information. Ask your supplier for a copy of this documentation including prescriptions.
The same thing may be true with your doctor’s office, a request for supplies may have been denied because the information needed was not given to the insurance company or supply company. So then you need to speak with someone to discover what was missing. Sometimes the problem can be found, corrected and then the supply company can resubmit with positive results.
If you receive a denial, you have the right to appeal. The appeal usually has a time limit attached so follow the instructions for an appeal and respond that you want to appeal the denial. If you have non-Medicare insurance you may be able to speak with someone at the insurance company about your denial to figure out why your request was denied as part of the appeal process. You may also contact your insurance customer service and request a case manager to assist with your supply denial.
If you have Medicare, for assistance you can contact your local representative from the Beneficiary of Family Centered Care – Quality Improvement Organization (BFCC-QIO) or call 1-800-MEDICARE to help you understand the appeal process and determine what is still missing from your record. Your supply company may also be able to help you.
Do You Know What’s in Your Medical Records?
You have a right to request a copy. In 1996 the Health Information Portability and Accountability Act (HIPPA) was passed. It is the law that protects patients’ health information from being shared with only those who have a need to know. It also states that patients are allowed access to their health records. Your medical record is not just your doctor’s office records, it includes hospital, nursing home, or home health agency (HHA) records, and records from other healthcare professionals including, but not limited to, nurses, therapists, and social workers. Here is a great video example of advocating for yourself and knowing what’s in your record.
Each state has its own laws about what is required to get copies of your medical records. Check with your medical provider/facility for their policy on obtaining your medical records.
Conclusion
To avoid claim denials, long appeal processes, costs to you, or the possibility of not receiving your ostomy supplies, you need to make sure that:
- Your supplier is submitting correct information and up to date medical records to your insurance company (or Medicare); and
- Your physician keeps up-to-date medical records about your health, your ostomy and your supplies in your medical record.
Just recently ostomy advocate Megan, The Front Butt YouTuber, tweeted, “Currently going through some of my medical records. Found several pieces of misinformation, which I cleared up in visits and it was marked incorrectly. Yet, they are still present on my record. Again, patients are NOT being listened to.” (9/4/18 Twitter) Kudos to her for taking an active role in her healthcare, and going through her medical records. Self-advocacy is ongoing and no doubt she will be bringing this up again until it is CORRECT!
Remember that you have the right to change physicians and the right to change your ostomy supply company if they are not working with you.
It’s time to take control of your health. You deserve high-quality care.